- Iron overload
-
Iron overload
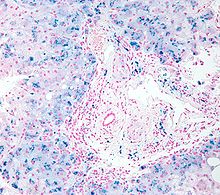
Micrograph of haemosiderosis. Liver biopsy. Iron stain.ICD-10 R79.0 ICD-9 xxx DiseasesDB 5581 MeSH D019190 In medicine, iron overload indicates accumulation of iron in the body from any cause. The most important causes are hereditary hemochromatosis (HHC), a genetic disease, and transfusional iron overload, which can result from repeated blood transfusion.
Contents
Terminology
Haemochromatosis or haemosiderosis
Historically, the term haemochromatosis (spelled hemochromatosis in American English) was initially used to refer to what is now more specifically called haemochromatosis type 1 (or HFE-related hereditary haemochromatosis). Currently, haemochromatosis (without further specification) is mostly defined as iron overload with a hereditary/primary cause,[1][2] or originating from a metabolic disorder.[3] However, the term is currently also used more broadly to refer to any form of iron overload, thus requiring specification of the cause, for example, hereditary haemochromatosis. Hereditary haemochromatosis is an autosomal recessive disease with estimated prevalence in the population of 2 in 1,000 among patients with European ancestry, with lower incidence in other ethnic groups. The gene responsible for hereditary haemochromatosis (known as HFE gene) is located on chromosome 6; the majority of hereditary haemochromatosis patients have mutations in this HFE gene. Hereditary haemochromatosis is characterized by an accelerated rate of intestinal iron absorption and progressive iron deposition in various tissues that typically begins to be expressed in the third to fifth decades of life, but may occur in children. The most common presentation is hepatic cirrhosis in combination with hypopituitarism, cardiomyopathy, diabetes, arthritis, or hyperpigmentation. Because of the severe sequelae of this disease if left untreated, and recognizing that treatment is relatively simple, early diagnosis before symptoms or signs appear is important.[4][5]
In general, the term haemosiderosis is used to indicate the pathological effect of iron accumulation in any given organ, which mainly occurs in the form of haemosiderin.[6][7] Sometimes, the simpler term siderosis is used instead.
Other definitions distinguishing haemochromatosis or haemosiderosis that are occasionally used include:
- Haemosiderosis is haemochromatosis caused by excessive blood transfusions, that is, haemosiderosis is a form of secondary haemochromatosis.[8][9]
- Haemosiderosis is hemosiderin deposition within cells, while haemochromatosis is hemosiderin within cells and interstitium.[10]
- Haemosiderosis is iron overload that does not cause tissue damage,[11] while haemochromatosis does.[12]
- Haemosiderosis is arbitrarily differentiated from haemochromatosis by the reversible nature of the iron accumulation in the reticuloendothelial system.[13]
Clinical presentation
Organs commonly affected by haemochromatosis are the liver, heart, and endocrine glands.[14]
Haemochromatosis may present with the following clinical syndromes:[15]
- Cirrhosis of the liver
- Diabetes due to pancreatic islet cell failure
- Cardiomyopathy
- Arthritis (iron deposition in joints)
- Testicular failure
- Tanning of the skin
Causes
The causes can be distinguished between primary cases (hereditary or genetically determined) and less frequent secondary cases (acquired during life).[16] People of Celtic (Irish, Scottish, Welsh) origin have a particularly high incidence of whom about 10% are carriers of the gene and 1% sufferers from the condition.
Primary haemochromatosis
The fact that most cases of haemochromatosis were inherited was well known for most of the 20th century, though they were incorrectly assumed to depend on a single gene.[17] The overwhelming majority actually depend on mutations of the HFE gene discovered in 1996, but since then others have been discovered and sometimes are grouped together as "non-classical hereditary haemochromatosis",[18] "non-HFE related hereditary haemochromatosis",[19] or "non-HFE haemochromatosis".[20]
Description OMIM Mutation haemochromatosis type 1: "classical" haemochromatosis 235200 HFE Haemochromatosis type 2A: juvenile haemochromatosis 602390 Haemojuvelin ("HJV", also known as RGMc and HFE2) Haemochromatosis type 2B: juvenile haemochromatosis 606464 hepcidin antimicrobial peptide (HAMP) or HFE2B Haemochromatosis type 3 604250 transferrin receptor-2 (TFR2 or HFE3) Haemochromatosis type 4/
African iron overload604653 ferroportin (SLC11A3/SLC40A1) Neonatal haemochromatosis 231100 (unknown) Acaeruloplasminemia (very rare) 604290 caeruloplasmin Congenital atransferrinaemia (very rare) 209300 transferrin GRACILE syndrome (very rare) 603358 BCS1L Most types of hereditary haemochromatosis have autosomal recessive inheritance, while type 4 has autosomal dominant inheritance.[21]
Secondary haemochromatosis
- Severe chronic haemolysis of any cause, including intravascular haemolysis and ineffective erythropoiesis (haemolysis within the bone marrow).
- Multiple frequent blood transfusions (either whole blood or just red blood cells), which are usually needed either by individuals with hereditary anaemias (such as beta-thalassaemia major, sickle cell anaemia, and Diamond–Blackfan anaemia) or by older patients with severe acquired anaemias such as in myelodysplastic syndromes.
- Excess parenteral iron supplements, such as can acutely happen in iron poisoning
- Excess dietary iron
- Some disorders do not normally cause haemochromatosis on their own, but may do so in the presence of other predisposing factors. These include cirrhosis (especially related to alcohol abuse), steatohepatitis of any cause, porphyria cutanea tarda, prolonged haemodialysis, post-portacaval shunting.
Diagnosis
There are several methods available for diagnosing and monitoring iron loading including:
- Serum ferritin
- Liver biopsy
- HFE
- MRI
Serum ferritin is a low-cost, readily available, and minimally invasive method for assessing body iron stores. However, the major problem with using it as an indicator of iron overload is that it can be elevated in a range of other medical conditions unrelated to iron levels including infection, inflammation, fever, liver disease, renal disease, and cancer. Also, total iron binding capacity may be low, but can also be normal.[22]
The standard of practice in diagnosis of hemochromatosis was recently reviewed by Pietrangelo.[4] Positive HFE analysis confirms the clinical diagnosis of hemochromatosis in asymptomatic individuals with blood tests showing increased iron stores, or for predictive testing of individuals with a family history of hemochromatosis. The alleles evaluated by HFE gene analysis are evident in ~80% of patients with hemochromatosis; a negative report for HFE gene does not rule out hemochromatosis. In a patient with negative HFE gene testing, elevated iron status for no other obvious reason, and family history of liver disease, additional evaluation of liver iron concentration is indicated. In this case, diagnosis of hemochromatosis is based on biochemical analysis and histologic examination of a liver biopsy. Assessment of the hepatic iron index (HII) is considered the "gold standard" for diagnosis of hemochromatosis.
MRI is emerging as an alternative to liver biopsy for measuring liver iron loading. For measuring liver iron concentrations, R2-MRI (also known as FerriScan) [1][23] has been extensively validated. More than 11,000 FerriScans have now been conducted in over 120 medical centres across 25 countries. FerriScan is now specifically recommended as a method to measure liver iron concentrations in clinical practice guidelines for thalassemias,[24][25][26][27][28] sickle cell disease [29][30][31] myelodysplastic syndrome (MDS) [32][33][34] and hereditary hemochromatosis.[35]
Family members of those diagnosed with primary hemochromatosis may be advised to be screened genetically to determine if they are a carrier or if they could develop the disease. This can allow preventative measures to be taken.
Prognosis
A third of those untreated develop hepatocellular carcinoma.[36]
Treatment
Routine treatment in an otherwise-healthy person consists of regularly scheduled phlebotomies (bloodletting). When first diagnosed, the phlebotomies may be fairly frequent, perhaps as often as once a week, until iron levels can be brought to within normal range. Once iron and other markers are within the normal range, phlebotomies may be scheduled every other month or every three months depending upon the patient's rate of iron loading.
For those unable to tolerate routine blood draws, there is a chelating agent available for use. The drug Deferoxamine binds with iron in the bloodstream and enhances its elimination via urine and faeces. Typical treatment for chronic iron overload requires subcutaneous injection over a period of 8–12 hours daily. Two newer iron chelating drugs that are licensed for use in patients receiving regular blood transfusions to treat thalassemia (and, thus, who develop iron overload as a result) are deferasirox and deferiprone.
See also
References
- ^ thefreedictionary.com > hemochromatosis, citing:
- The American Heritage Medical Dictionary, 2004 by Houghton Mifflin Company
- McGraw-Hill Concise Dictionary of Modern Medicine. 2002
- ^ Merriam-Webster's Medical Dictionary > hemochromatosis Retrieved on Dec 11, 2009
- ^ thefreedictionary.com, citing:
- Dorland's Medical Dictionary for Health Consumers, 2007
- Mosby's Medical Dictionary, 8th edition. 2009
- Jonas: Mosby's Dictionary of Complementary and Alternative Medicine. 2005,
- ^ a b Pietrangelo, Antonello (2010). "Hereditary Hemochromatosis: Pathogenesis, Diagnosis, and Treatment". Gastroenterology 139 (2): 393–408. doi:10.1053/j.gastro.2010.06.013. PMID 20542038.
- ^ Brandhagen, D J; Fairbanks, V F; Batts, K P; Thibodeau, S N (1999). "Update on hereditary hemochromatosis and the HFE gene". Mayo Clinic Proceedings 74 (9): 917–21. doi:10.4065/74.9.917. PMID 10488796.
- ^ Merriam-Webster's Medical Dictionary > hemosideroses Retrieved on Dec 11, 2009
- ^ thefreedictionary.com > hemosiderosis, citing:
- The American Heritage Medical Dictionary, 2004 by Houghton Mifflin Company
- Mosby's Medical Dictionary, 8th edition.
- ^ eMedicine Specialties > Radiology > Gastrointestinal > Hemochromatosis Author: Sandor Joffe, MD. Updated: May 8, 2009
- ^ thefreedictionary.com > hemosiderosis, citing:
- Gale Encyclopedia of Medicine. Copyright 2008
- ^ Notecards on radiology gamuts, diseases, anatomy 2002, Charles E. Kahn, Jr., MD. Medical College of Wisconsin
- ^ thefreedictionary.com > hemosiderosis, citing:
- Dorland's Medical Dictionary for Health Consumers, 2007
- Mosby's Dental Dictionary, 2nd edition.
- Saunders Comprehensive Veterinary Dictionary, 3 ed. 2007
- ^ The HealthScout Network > Health Encyclopedia > Diseases and Conditions > Hemochromatosis Retrieved on Dec 11, 2009
- ^ thefreedictionary.com > hemosiderosis, citing:
- McGraw-Hill Concise Dictionary of Modern Medicine. 2002
- ^ Andrews, Nancy C. (1999). "Disorders of Iron Metabolism". New England Journal of Medicine 341 (26): 1986–95. doi:10.1056/NEJM199912233412607. PMID 10607817.
- ^ John Murtagh (2007). General Practice. McGraw Hill Australia. ISBN 0074704362.[page needed]
- ^ Pietrangelo, A (2003). "Haemochromatosis". Gut 52 (90002): ii23–30. doi:10.1136/gut.52.suppl_2.ii23. PMC 1867747. PMID 12651879. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1867747.
- ^ Cam Patterson; Marschall S. Runge (2006). Principles of molecular medicine. Totowa, NJ: Humana Press. pp. 567. ISBN 1-58829-202-9.
- ^ Mendes, Ana Isabel; Ferro, Ana; Martins, Rute; Picanço, Isabel; Gomes, Susana; Cerqueira, Rute; Correia, Manuel; Nunes, António Robalo et al. (2008). "Non-classical hereditary hemochromatosis in Portugal: novel mutations identified in iron metabolism-related genes". Annals of Hematology 88 (3): 229–34. doi:10.1007/s00277-008-0572-y. PMID 18762941.
- ^ Maddrey, Willis C.; Schiff, Eugene R.; Sorrell, Michael F. (2007). Schiff's diseases of the liver. Hagerstwon, MD: Lippincott Williams & Wilkins. pp. 1048. ISBN 0-7817-6040-2.
- ^ Pietrangelo, Antonello (2005). "Non-HFE Hemochromatosis". Seminars in Liver Disease 25 (4): 450–60. doi:10.1055/s-2005-923316. PMID 16315138.
- ^ Franchini, Massimo (2006). "Hereditary iron overload: Update on pathophysiology, diagnosis, and treatment". American Journal of Hematology 81 (3): 202–9. doi:10.1002/ajh.20493. PMID 16493621.
- ^ labtestsonline.org > TIBC & UIBC, Transferrin Last reviewed on October 28, 2009.
- ^ St. Pierre, T. G.; Clark, PR; Chua-Anusorn, W; Fleming, AJ; Jeffrey, GP; Olynyk, JK; Pootrakul, P; Robins, E et al. (2005). "Noninvasive measurement and imaging of liver iron concentrations using proton magnetic resonance". Blood 105 (2): 855–61. doi:10.1182/blood-2004-01-0177. PMID 15256427.
- ^ Cooley's Anemia Foundation 2010 Position Statement
- ^ TIF Guidelines for the Clinical Management of Thalassemia, 2nd Edition (www.thalassaemia.org.cy)
- ^ Standard for the Clinical Care of Children and Adults with Thalassemia in the UK (www.ukts.org)
- ^ Angelucci E, et al. Italian Society of Hematology practice guidelines for the management of iron overload in thalassemia major and related disorders. Haematologica 2008;93(5):741-752.
- ^ Taher A, et al. Correlation of liver iron concentration determined by R2 magnetic resonance imaging with serum ferritin in patients with thalassemia intermedia. Haematologica 2008;93(10):1584-1586
- ^ UK Standard of Care for Adults with Sickle Cell Disease (www.sicklecellsociety.org)
- ^ NIH Guidelines (www.nhlbi.nih.gov)
- ^ Nursing Practice Guidelines: Care of Patients with sickle cell disease and iron overload. International Association of Sickle Cell Nurses and Physician Assistants. 2008
- ^ Wells, R.A., et al., Iron overload in myelodysplastic syndromes: a Canadian consensus guideline. Leuk Res, 2008. 32(9): p. 1338-53.
- ^ Bennett, J.M., Consensus statement on iron overload in myelodysplastic syndromes. Am J Hematol, 2008. 83(11): p. 858-61.
- ^ Suzuki, T., et al., Japanese epidemiological survey with consensus statement on Japanese guidelines for treatment of iron overload in bone marrow failure syndromes. Int J Hematol, 2008. 88(1): p. 30-5.
- ^ European Association For The Study Of The Liver., EASL clinical practice guidelines for HFE hemochromatosis. J Hepatol, 2010. 53(1): p. 3-22.
- ^ McLean, David I.; Harley A. Haynes (2003). "Chapter 184: Cutaneous Manifestations of Internal Malignant Disease: Cutaneous Paraneoplastic Syndromes". In Freedberg et al. Fitzpatrick's Dermatology in General Medicine. (6th ed.). McGraw-Hill. ISBN 0-07-138067-1.
External links
- FerriScan - MRI-based test to measure iron overload
- Iron Overload (Texas Medical Center)
- Iron Overload - Hemosiderosis - Hemochromatosis (Merck)
- Iron Overload.org
- UK Haemochromatosis Society
- haemochromatosis.org
- Haemochromatosis.org.au
- GeneReview/NCBI/NIH/UW entry on HFE-Associated Hereditary Hemochromatosis
- Haemochromatosis Society of South Africa
- Canadian Hemochromatosis Society
- GeneReview/NCBI/NIH/UW entry on TFR2-Related Hereditary Hemochromatosis
- GeneReview/NCBI/NIH/UW entry on Juvenile Hereditary Hemochromatosis
- GeneReview/NCBI/NIH/UW entry on Aceruloplasminemia
Inborn error of metal metabolism (E83, 275) Transition metal high: Primary iron overload disorder: Hemochromatosis/HFE1 · Juvenile/HFE2 · HFE3 · African iron overload/HFE4 · Aceruloplasminemia · Atransferrinemia · Hemosiderosisdeficiency: Iron deficiencyCuZnhigh: Zinc toxicitydeficiency: Acrodermatitis enteropathicaElectrolyte see Template:Water-electrolyte imbalance and acid-base imbalancehigh: Hyperphosphatemiahigh: Hypermagnesemiadeficiency: Hypomagnesemiahigh: Hypercalcaemia · Milk-alkali syndrome (Burnett's) · Calcinosis (Calciphylaxis, Calcinosis cutis) · Calcification (Metastatic calcification, Dystrophic calcification) · Familial hypocalciuric hypercalcemiaM: NUT
cof, enz, met
noco, nuvi, sysi/epon, met
drug(A8/11/12)
Abnormal clinical and laboratory findings for blood tests (R70–R79, 790) Red blood cells SizeShape (Poikilocyte)developmental organelles (Howell-Jolly body, Basophilic stippling, Pappenheimer bodies, Cabot rings)abnormal hemoglobin precipitation (Heinz body)OtherLymphocytes Smudge cell · Downey cellSmall molecules NitrogenousProteins OtherElevated cardiac markers · Elevated alpha-fetoproteinMinerals Iron overload disorderPathogens/sepsis Categories:- Inborn errors of metal metabolism
- Abnormal clinical and laboratory findings for blood
Wikimedia Foundation. 2010.