- Beta blocker
-
Beta blockers Drug class 
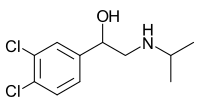
Skeletal formula of propranolol, the first clinically successful beta blockerATC code C07 MeSH D000319 AHFS/Drugs.com list of generics Consumer Reports best-buy-drugs WebMD medicinenet rxlist Biological target beta receptors Beta blockers (sometimes written as β-blockers) or beta-adrenergic blocking agents, beta-adrenergic antagonists, beta-adrenoreceptor antagonists or beta antagonists, are a class of drugs used for various indications. They are particularly for the management of cardiac arrhythmias, cardioprotection after myocardial infarction[1] (heart attack), and hypertension.[2] As beta adrenergic receptor antagonists, they diminish the effects of epinephrine (adrenaline) and other stress hormones. In 1958 the first beta blocker, dichloroisoproterenol, was synthesised by Eli Lilly Laboratories,[3] but it was Sir James W. Black in 1962,[4] who found the first clinically significant use of beta blockers with propranolol and pronethalol; it revolutionized the medical management of angina pectoris[5] and is considered by many to be one of the most important contributions to clinical medicine and pharmacology of the 20th century.[6]
Beta blockers block the action of endogenous catecholamines epinephrine (adrenaline) and norepinephrine (noradrenaline) in particular, on β-adrenergic receptors, part of the sympathetic nervous system which mediates the "fight or flight" response.[7][8] There are three known types of beta receptor, designated β1, β2 and β3 receptors.[9] β1-adrenergic receptors are located mainly in the heart and in the kidneys.[8] β2-adrenergic receptors are located mainly in the lungs, gastrointestinal tract, liver, uterus, vascular smooth muscle, and skeletal muscle.[8] β3-adrenergic receptors are located in fat cells.[10]
Contents
Medical uses
Large differences exist in the pharmacology of agents within the class, thus not all beta blockers are used for all indications listed below.
Indications for beta blockers include:
- Angina pectoris
- Atrial fibrillation
- Cardiac arrhythmia
- Congestive heart failure
- Essential tremor
- Glaucoma
- Hypertension
- Migraine prophylaxis
- Mitral valve prolapse
- Myocardial infarction
- Phaeochromocytoma, in conjunction with α-blocker
- Postural orthostatic tachycardia syndrome
- Symptomatic control (tachycardia, tremor) in anxiety and hyperthyroidism
Beta blockers have also been used in the following conditions:
- Acute aortic dissection
- Hypertrophic obstructive cardiomyopathy
- Marfan syndrome (treatment with propranolol slows progression of aortic dilation and its complications)
- Prevention of variceal bleeding in portal hypertension
- Possible mitigation of hyperhidrosis
- Social anxiety disorder and other anxiety disorders
Congestive heart failure
Although beta blockers were once contraindicated in congestive heart failure, as they have the potential to worsen the condition, studies in the late 1990s showed their efficacy at reducing morbidity and mortality in congestive heart failure.[11][12][13] Bisoprolol, carvedilol and sustained-release metoprolol are specifically indicated as adjuncts to standard ACE inhibitor and diuretic therapy in congestive heart failure.
Beta blockers are primarily known for their reductive effect on heart rate, although this is not the only mechanism of action of importance in congestive heart failure[citation needed]. Beta blockers, in addition to their sympatholytic B1 activity in the heart, influence the renin/angiotensin system at the kidneys. Beta blockers cause a decrease in renin secretion, which in turn reduce the heart oxygen demand by lowering extracellular volume and increasing the oxygen carrying capacity of blood. Beta blockers sympatholytic activity reduce heart rate, thereby increasing the ejection fraction of the heart despite an initial reduction in ejection fraction.
Trials have shown that beta blockers reduce the absolute risk of death by 4.5% over a 13 month period. As well as reducing the risk of mortality, the number of hospital visits and hospitalizations were also reduced in the trials.[14]
Anxiety and performance enhancement
There is clear evidence from many controlled trials in the past 25 years that beta blockers are effective in anxiety disorders, though the mechanism of action is not known.[15] Some people have used beta blockers for performance enhancement, and especially to combat performance anxiety. In particular, musicians, public speakers, actors, and professional dancers, have been known to use beta blockers to avoid stage fright and tremor during public performance and especially auditions.
The application to stage fright was first recognized in The Lancet in 1976 and by 1987, a survey conducted by the International Conference of Symphony Orchestra Musicians, representing the 51 largest orchestras in the United States, revealed that 27 percent of its musicians had used beta blockers and that 70 percent obtained them from friends, not physicians.[16] Beta blockers are inexpensive, said to be relatively safe and, on one hand, seem to improve musicians performances on a technical level while some say the performance may be perceived as "soulless and inauthentic".[16]
The physiological symptoms of the fight/flight response associated with performance anxiety and panic (pounding heart, cold/clammy hands, increased respiration, sweating, etc.) are significantly reduced, thus enabling anxious individuals to concentrate on the task at hand. Stutterers also use beta blockers to avoid fight/flight responses, hence reducing the tendency to stutter. Officially, beta blockers are not approved for anxiolytic use by the U.S. Food and Drug Administration.[17]
Since they promote a lower heart rate and reduce tremor, beta blockers have been used by some Olympic marksmen to enhance performance, though beta blockers are banned by the International Olympic Committee (IOC).[18] Although they have no recognisable benefit to most sports, it is acknowledged that they are beneficial to sports such as archery and shooting. A recent, high-profile transgression took place in the 2008 Summer Olympics, where 50 metre pistol silver medallist and 10 metre air pistol bronze medallist Kim Jong-su tested positive for propranolol and was stripped of his medal.
Preventing PTSD
Posttraumatic stress disorder (PTSD) is theorized to be the result of neurological patterns caused by adrenaline and fear in the brain. By administering beta blockers immediately following a traumatic event, as well as over the next couple weeks, the formation of PTSD has been reduced in clinical studies.[citation needed]
Adverse effects
Adverse drug reactions (ADRs) associated with the use of beta blockers include: nausea, diarrhoea, bronchospasm, dyspnea, cold extremities, exacerbation of Raynaud's syndrome, bradycardia, hypotension, heart failure, heart block, fatigue, dizziness, alopecia (hair loss), abnormal vision, hallucinations, insomnia, nightmares, sexual dysfunction, erectile dysfunction and/or alteration of glucose and lipid metabolism. Mixed α1/β-antagonist therapy is also commonly associated with orthostatic hypotension. Carvedilol therapy is commonly associated with edema.[19]
Central nervous system (CNS) adverse effects (hallucinations, insomnia, nightmares) are more common in agents with greater lipid solubility, which are able to cross the blood-brain barrier into the CNS. Similarly, CNS adverse effects are less common in agents with greater aqueous solubility (listed below).
Adverse effects associated with β2-adrenergic receptor antagonist activity (bronchospasm, peripheral vasoconstriction, alteration of glucose and lipid metabolism) are less common with β1-selective (often termed "cardioselective") agents, however receptor selectivity diminishes at higher doses. Beta blockade, especially of the beta-1 receptor at the macula densa inhibits renin release, thus decreasing the release of aldosterone. This causes hyponatremia and hyperkalemia.
Hypoglycemia can occur with beta-blockade because β2-adrenoceptors normally stimulate hepatic glycogen breakdown (glycogenolysis) and pancreatic release of glucagon, which work together to increase plasma glucose. Therefore, blocking β2-adrenoceptors lowers plasma glucose. β1-blockers have fewer metabolic side effects in diabetic patients; however, the tachycardia which serves as a warning sign for insulin-induced hypoglycemia may be masked. Therefore, beta-blockers are to be used cautiously in diabetics. [20]
A 2007 study revealed that diuretics and beta-blockers used for hypertension increase a patient's risk of developing diabetes while ACE inhibitors and Angiotensin II receptor antagonists (Angiotensin Receptor Blockers) actually decrease the risk of diabetes.[21] Clinical guidelines in Great Britain, but not in the United States, call for avoiding diuretics and beta-blockers as first-line treatment of hypertension due to the risk of diabetes.[22]
Beta blockers must not be used in the treatment of cocaine, amphetamine, or other alpha adrenergic stimulant overdose. The blockade of only beta receptors increases hypertension, reduces coronary blood flow, left ventricular function, and cardiac output and tissue perfusion by means of leaving the alpha adrenergic system stimulation unopposed.[23] The appropriate antihypertensive drugs to administer during hypertensive crisis resulting from stimulant abuse are vasodilators like nitroglycerin, diuretics like furosemide and alpha blockers like phentolamine.[24]
Contraindications
They are contraindicative to patients with asthma as stated in the BNF 2011. Beta blockers should also be avoided in patients with history of cocaine use or in cocaine-induced tachycardia or MI.
Toxicity
Glucagon has been used in the treatment of overdose.[25][26] Glucagon has a positive inotropic action on the heart and decreases renal vascular resistance. It is therefore useful in patients with beta-blocker cardiotoxicity. Glucagon is the specific antidote for beta-blocker poisoning, because it increases intracellular cAMP and cardiac contractility. [27] [28] Cardiac pacing should be reserved for patients unresponsive to pharmacological therapy.
Patients who experience bronchospasm due to the B2 blocking effects of non-selective beta-blockers may be treated with anticholinergic drugs such as Ipratropium, which are safer than beta agonists in patients with cardiovascular disease.
β-Receptor antagonism
Stimulation of β1 receptors by epinephrine induces a positive chronotropic and inotropic effect on the heart and increases cardiac conduction velocity and automaticity.[29] Stimulation of β1 receptors on the kidney causes renin release.[30] Stimulation of β2 receptors induces smooth muscle relaxation,[31] induces tremor in skeletal muscle,[32] and increases glycogenolysis in the liver and skeletal muscle.[33] Stimulation of β3 receptors induces lipolysis.[34]
Beta blockers inhibit these normal epinephrine-mediated sympathetic actions,[7] but have minimal effect on resting subjects[citation needed]. That is, they reduce excitement/physical exertion on heart rate and force of contraction,[35] and also tremor[36] and breakdown of glycogen, but increase dilation of blood vessels[37] and constriction of bronchi.[38]
It is therefore expected that non-selective beta blockers have an antihypertensive effect.[39] The primary antihypertensive mechanism of betablockers is unclear but it may involve reduction in cardiac output (due to negative chronotropic and inotropic effects).[40] It may also be due to reduction in renin release from the kidneys, and a central nervous system effect to reduce sympathetic activity (for those β-blockers that do cross the blood-brain barrier, e.g. Propranolol).
Antianginal effects result from negative chronotropic and inotropic effects, which decrease cardiac workload and oxygen demand. Negative chronotropic properties of beta blockers allow the lifesaving property of heart rate control. Beta blockers are readily titrated to optimal rate control in many pathologic states.
The antiarrhythmic effects of beta blockers arise from sympathetic nervous system blockade – resulting in depression of sinus node function and atrioventricular node conduction, and prolonged atrial refractory periods. Sotalol, in particular, has additional antiarrhythmic properties and prolongs action potential duration through potassium channel blockade.
Blockade of the sympathetic nervous system on renin release leads to reduced aldosterone via the renin angiotensin aldosterone system with a resultant decrease in blood pressure due to decreased sodium and water retention.
Intrinsic sympathomimetic activity
Also referred to as intrinsic sympathomimetic effect, this term is used particularly with beta blockers that can show both agonism and antagonism at a given beta receptor, depending on the concentration of the agent (beta blocker) and the concentration of the antagonized agent (usually an endogenous compound such as norepinephrine). See partial agonist for a more general description.
Some beta blockers (e.g. oxprenolol, pindolol, penbutolol and acebutolol) exhibit intrinsic sympathomimetic activity (ISA). These agents are capable of exerting low level agonist activity at the β-adrenergic receptor while simultaneously acting as a receptor site antagonist. These agents, therefore, may be useful in individuals exhibiting excessive bradycardia with sustained beta blocker therapy.
Agents with ISA are not used in post-myocardial infarction as they have not been demonstrated to be beneficial. They may also be less effective than other beta blockers in the management of angina and tachyarrhythmia.[19]
α1-Receptor antagonism
Some beta blockers (e.g. labetalol and carvedilol) exhibit mixed antagonism of both β- and α1-adrenergic receptors, which provides additional arteriolar vasodilating action.
Other effects
Beta blockers decrease nocturnal melatonin release, perhaps partly accounting for sleep disturbance caused by some agents.[41]
They can also be used to treat glaucoma because they decrease intraocular pressure by lowering aqueous humor secretion.[42]
Examples of beta blockers
Non-selective agents
- Alprenolol
- Bucindolol
- Carteolol
- Carvedilol (has additional α-blocking activity)
- Labetalol (has additional α-blocking activity)
- Nadolol
- Oxprenolol
- Penbutolol (has intrinsic sympathomimetic activity)
- Pindolol (has intrinsic sympathomimetic activity)
- Propranolol
- Sotalol
- Timolol
- Eucommia bark (herb)
β1-Selective agents
- Acebutolol (has intrinsic sympathomimetic activity)
- Atenolol
- Betaxolol
- Bisoprolol
- Celiprolol
- Esmolol[43]
- Metoprolol
- Nebivolol
β2-Selective agents
- Butaxamine (weak α-adrenergic agonist activity) - No common clinical applications, but used in experiments.
- ICI-118,551 Highly selective β2-adrenergic receptor antagonist - No known clinical applications, but used in experiments due to its strong receptor specificity.
β3-Selective agents
- SR 59230A (has additional α-blocking activity) - Used in experiments.
Comparative information
Pharmacological differences
- Agents with intrinsic sympathomimetic action (ISA)
- Acebutolol, carteolol, celiprolol, mepindolol, oxprenolol, pindolol, labetalol.
- Agents with greater aqueous solubility (hydrophilic beta blockers)
- Atenolol, celiprolol, nadolol, sotalol
- Agents with membrane stabilizing effect
- Acebutolol, betaxolol, pindolol, propranolol
- Agents with antioxidant effect
- Carvedilol, nebivolol
Indication differences
- Agents specifically indicated for cardiac arrhythmia
- Agents specifically indicated for congestive heart failure
- Agents specifically indicated for glaucoma
- Agents specifically indicated for myocardial infarction
- Agents specifically indicated for migraine prophylaxis
Propranolol is the only agent indicated for control of tremor, portal hypertension, and esophageal variceal bleeding, and used in conjunction with α-blocker therapy in phaeochromocytoma.[19]
See also
- Alpha blockers
References
- ^ Freemantle N, Cleland J, Young P, Mason J, Harrison J (June 1999). "beta Blockade after myocardial infarction: systematic review and meta regression analysis". BMJ 318 (7200): 1730–7. PMC 31101. PMID 10381708. http://bmj.com/cgi/pmidlookup?view=long&pmid=10381708. Retrieved 2010-09-06.
- ^ Cruickshank JM (August 2010). "Beta blockers in hypertension". Lancet 376 (9739): 415; author reply 415–6. doi:10.1016/S0140-6736(10)61217-2. PMID 20692524. http://linkinghub.elsevier.com/retrieve/pii/S0140-6736(10)61217-2. Retrieved 2010-09-06.
- ^ [|William H. Frishman] (2008-12). "Fifty years of beta-blockers: a revolution in CV pharmacotherapy". Cardiology Today. http://www.cardiologytoday.com/view.aspx?rid=33841. Retrieved 2010-09-06.
- ^ "Sir James Black inventor of beta-blockers passes away". http://www.news-medical.net/news/20100323/Sir-James-Black-inventor-of-beta-blockers-passes-away.aspx. Retrieved 2010-09-06.
- ^ van der Vring JA (June 1999). "Combination of calcium channel blockers and beta blockers for patients with exercise-induced angina pectoris: a double-blind parallel-group comparison of different classes of calcium channel blockers. The Netherlands Working Group on Cardiovascular Research (WCN)". Angiology 50 (6): 447–454. doi:10.1177/000331979905000602. PMID 10378820. http://ang.sagepub.com/cgi/pmidlookup?view=long&pmid=10378820. Retrieved 2010-09-06.
- ^ Stapleton MP (1997). "Sir James Black and propranolol. The role of the basic sciences in the history of cardiovascular pharmacology". Texas Heart Institute Journal / from the Texas Heart Institute of St. Luke's Episcopal Hospital, Texas Children's Hospital 24 (4): 336–42. PMC 325477. PMID 9456487. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=325477.
- ^ a b Frishman W.H.; Cheng-Lai A, Nawarskas J (2005). Current Cardiovascular Drugs. Current Science Group. pp. 152. ISBN 9781573402217. http://books.google.com/?id=y3R1Vd3NHqcC&pg=PA152&dq=mode+of+action+of+beta+blockers#v=onepage&q=mode%20of%20action%20of%20beta%20blockers&f=false. Retrieved 2010-09-07.
- ^ a b c Arcangelo V.P.; Peterson A.M. (2006). Pharmacotherapeutics for advanced practice: a practical approach. Lippincott Williams & Wilkins. pp. 205. ISBN 9780781757843. http://books.google.com/?id=EaP1yJz4fkEC&pg=PA205&dq=beta+receptors+heart+kidneys#v=onepage&q=beta%20receptors%20heart%20kidneys&f=false. Retrieved 2010-09-07.
- ^ Frishman W.H.; Cheng-Lai A, Nawarskas J (2005). Current Cardiovascular Drugs. Current Science Group. pp. 153. ISBN 9781573402217. http://books.google.com/?id=y3R1Vd3NHqcC&pg=PA152&dq=mode+of+action+of+beta+blockers#v=onepage&q=mode%20of%20action%20of%20beta%20blockers&f=false. Retrieved 2010-09-07.
- ^ Clément K, Vaisse C, Manning BS, Basdevant A, Guy-Grand B, Ruiz J, Silver KD, Shuldiner AR, Froguel P, Strosberg AD (August 1995). "Genetic variation in the beta 3-adrenergic receptor and an increased capacity to gain weight in patients with morbid obesity". The New England Journal of Medicine 333 (6): 352–354. doi:10.1056/NEJM199508103330605. PMID 7609752. http://www.nejm.org/doi/abs/10.1056/NEJM199508103330605. Retrieved 2010-09-07.
- ^ Hjalmarson A, Goldstein S, Fagerberg B et al. (2000). "Effects of controlled-release metoprolol on total mortality, hospitalizations, and well-being in patients with heart failure: the Metoprolol CR/XL Randomized Intervention Trial in congestive heart failure (MERIT-HF). MERIT-HF Study Group". JAMA 283 (10): 1295–1302. doi:10.1001/jama.283.10.1295. PMID 10714728.
- ^ Leizorovicz A, Lechat P, Cucherat M, Bugnard F (2002). "Bisoprolol for the treatment of chronic heart failure: a meta-analysis on individual data of two placebo-controlled studies--CIBIS and CIBIS II. Cardiac Insufficiency Bisoprolol Study". Am. Heart J. 143 (2): 301–307. doi:10.1067/mhj.2002.120768. PMID 11835035.
- ^ Packer M, Fowler MB, Roecker EB et al. (2002). "Effect of carvedilol on the morbidity of patients with severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) study". Circulation 106 (17): 2194–2199. doi:10.1161/01.CIR.0000035653.72855.BF. PMID 12390947.
- ^ Pritchett AM, Redfield MM (2002). "Beta-blockers: new standard therapy for heart failure" (PDF). Mayo Clin. Proc. 77 (8): 839–846. doi:10.4065/77.8.839. PMID 12173717. http://www.mayoclinicproceedings.com/pdf%2F7708%2F7708crc%2Epdf.
- ^ Tryer, Peter. "Anxiolytics not acting at the benzodiazepine receptor: Beta blockers." Progress in Neuro-Psychopharmacology and Biological Psychiatry. Volume 16, Issue 1, January 1992, Pages 17-26.
- ^ a b Blair Tindall. "Better Playing Through Chemistry", The New York Times, 17 October 2004. Retrieved 3 July 2011.
- ^ Schneier FR (2006). "Clinical practice. Social anxiety disorder". N. Engl. J. Med. 355 (10): 1029–1036. doi:10.1056/NEJMcp060145. PMID 16957148.
- ^ World Anti-Doping Agency (2005-09-19). "The Worl Anti-Doping Code: The 2006 Prohibited List International Standard". World Anti-Doping Agency. http://multimedia.olympic.org/pdf/en_report_1037.pdf. Retrieved 2006-12-13.
- ^ a b c Editor Rossi S, ed (2006). Australian Medicines Handbook. Adelaide: Australian Medicines Handbook.
- ^ Beta-Adrenoceptor Antagonists (Beta-Blockers); http://www.cvpharmacology.com/cardioinhibitory/beta-blockers.htm
- ^ Elliott WJ, Meyer PM (2007). "Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis". Lancet 369 (9557): 201–207. doi:10.1016/S0140-6736(07)60108-1. PMID 17240286.
- ^ Mayor S (2006). "NICE removes beta blockers as first line treatment for hypertension". BMJ 333 (7557): 8–8. doi:10.1136/bmj.333.7557.8-a. PMC 1488775. PMID 16809680. http://www.bmj.com/cgi/content/full/333/7557/8-a.
- ^ eMedicine - Toxicity, Cocaine : Article by Carlos J Roldan
- ^ eMedicine - Toxicity, Amphetamine : Article by Neal Handly
- ^ Weinstein RS, Cole S, Knaster HB, Dahlbert T (February 1985). "Beta blocker overdose with propranolol and with atenolol". Ann Emerg Med 14 (2): 161–163. doi:10.1016/S0196-0644(85)81081-7. PMID 2857542. http://linkinghub.elsevier.com/retrieve/pii/S0196-0644(85)81081-7.
- ^ "Toxicity, Beta-blocker: Treatment & Medication - eMedicine Emergency Medicine". http://emedicine.medscape.com/article/813342-treatment. Retrieved 2009-03-06.
- ^ Beta-Adrenergic Blocker Poisoning; http://www.courses.ahc.umn.edu/pharmacy/6124/handouts/Beta%20blockers.pdf
- ^ USMLE WORLD 2009 Step1, Pharmacology, Q85
- ^ [|Perez, Dianne M.] (2006). The Adrenergic Receptors In the 21st Century. Humana Press Inc.. p. 135. ISBN 1588294234. http://books.google.com/?id=QNpIsKwp8PUC&pg=PA135&dq=%CE%B21+receptors+positive+chronotropic+inotropic+effect#v=onepage&q=%CE%B21%20receptors%20positive%20chronotropic%20inotropic%20effect&f=false. Retrieved 2010-09-08.
- ^ [|Jameson, J. Larry]; [|Loscalzo, Joseph] (2010). Harrison's Nephrology and Acid-Base Disorders. McGraw-Hill Companies, Inc.. p. 215. ISBN 0071663398. http://books.google.com/?id=zVQZpJnQM_AC&pg=PA215&dq=%CE%B21+receptors+kidneys+renin#v=onepage&q&f=false. Retrieved 2010-09-08.
- ^ [|O'Donnell, John M.]; Nácul, Flávio E. (2009). Surgical Intensive Care Medicine. Springer. p. 47. ISBN 0387778926. http://books.google.com/?id=Bih5AXq_0uMC&pg=PA47&dq=b2+receptors+smooth+muscle+relaxation#v=onepage&q=b2%20receptors%20smooth%20muscle%20relaxation&f=false. Retrieved 2010-09-08.
- ^ Ahrens RC (1990). "Skeletal muscle tremor and the influence of adrenergic drugs". The Journal of Asthma : Official Journal of the Association for the Care of Asthma 27 (1): 11–20. PMID 1968452.
- ^ Reents, Stan (2000). Sport and exercise pharmacology. Human Kinetics. p. 19. ISBN 0873229371. http://books.google.com/?id=8ysOZlGnkC0C&pg=PA19&dq=beta+blocker+stimulation+glycogenolysis#v=onepage&q=beta%20blocker%20stimulation%20glycogenolysis&f=false. Retrieved 2010-09-10.
- ^ Martini, Frederic H. (2005). Anatomy and Physiology. Pearson Education. p. 394. ISBN 0805359478. http://books.google.com/?id=0e08PrEMQJoC&pg=PA394&dq=beta+3+stimulating+lipolysis#v=onepage&q=beta%203%20stimulating%20lipolysis&f=false. Retrieved 2010-09-10.
- ^ Khan, M. I. Gabriel (2006). Encyclopedia of Heart Diseases. Elsevier. p. 160. ISBN 0124060616. http://books.google.com/?id=xco9aJ_Y9XIC&pg=PA160&dq=beta+blockers+effects+on+heart+rate#v=onepage&q=beta%20blockers%20effects%20on%20heart%20rate&f=false. Retrieved 2010-09-10.
- ^ Lamster, Ira B.; [|Northridge, Mary E.], eds (2008). Improving Oral Health for the Elderly: An Interdisciplinary Approach. New York: Springer. p. 87. ISBN 9780387743370. http://books.google.com/?id=qs2v9Sm-dVoC&pg=PA87&dq=beta+blockers+reduce+tremor#v=onepage&q=beta%20blockers%20reduce%20tremor&f=false. Retrieved 2010-10-23.
- ^ Manger, William Muir; Gifford, Ray Wallace (2001). 100 Questions and Answers about Hypertension. Blackwell Science. p. 106. ISBN 0632044810. http://books.google.com/?id=DYFlmMeIVrIC&pg=PA106&dq=beta+blockers+dilation+of+blood+vessels#v=onepage&q=beta%20blockers%20dilation%20of%20blood%20vessels&f=false. Retrieved 2010-09-10.
- ^ Rothfeld, Glenn S.; Romaine, Deborah S. (2005). The Encyclopedia of Men's Health. Amaranth. p. 48. ISBN 0816051771. http://books.google.com/?id=AyPacn1o4nIC&pg=PA48&dq=beta+blockers+opening+of+bronchi#v=onepage&q&f=false. Retrieved 2010-10-23.
- ^ [|Hurst, J.W.] (1997). Schlant, Robert C.. ed. Hurst's the Heart. 2. Blackwell Science.. p. 1564. ISBN 007912951X. http://books.google.com/?id=eWQAJDrVV7gC&pg=PA1564&dq=beta+blockers+antihypertensive#v=onepage&q=beta%20blockers%20antihypertensive&f=false. Retrieved 2010-10-07.
- ^ Reid, J.L. (2001). Lecture notes on clinical pharmacology. 6. Blackwell Science.. p. 76. ISBN 0632050772. http://books.google.com/?id=dsEmlotDt2wC&pg=PA76&dq=beta+blockers+antihypertensive+effect+reduction+of+cardiac+output#v=onepage&q=beta%20blockers%20antihypertensive%20effect%20reduction%20of%20cardiac%20output&f=false. Retrieved 2011-03-11.
- ^ Stoschitzky K, Sakotnik A, Lercher P et al. (1999). "Influence of beta-blockers on melatonin release". Eur. J. Clin. Pharmacol. 55 (2): 111–115. doi:10.1007/s002280050604. PMID 10335905.
- ^ Shen, Howard (2008). Illustrated Pharmacology Memory Cards: PharMnemonics. Minireview. pp. 15. ISBN 1-59541-101-1.
- ^ Umehara S, Goyagi T, Nishikawa T, Tobe Y, Masaki Y (2010). "Esmolol and landiolol, selective beta1-adrenoreceptor antagonists, provide neuroprotection against spinal cord ischemia and reperfusion in rats". Anesthesia and Analgesia 21 (3): 1133–7. doi:10.1213/ANE.0b013e3181cdb06b. PMID 20103544. http://www.ncbi.nlm.nih.gov/pubmed/20103544.
External links
- Musicians and beta-blockers by Gerald Klickstein, March 11, 2010 (A blog post that considers "whether beta-blockers are safe, effective, and appropriate for performers to use.")
- Better Playing Through Chemistry by Blair Tindall, New York Times, October 17, 2004. (Discusses the use of beta blockers among professional musicians)
- Musicians using beta blockers by Blair Tindall. Condensed version of above article.
- In Defense of the Beta Blocker by Carl Elliott, The Atlantic, August 20, 2008. (Discusses the use of propranolol by a North Korean pistol shooter in the 2008 Olympics)
- MeSH beta-Adrenergic+Blockers
Sympatholytic (and closely related) antihypertensives (C02) Sympatholytics
(antagonize α-adrenergic
vasoconstriction)CentralAdrenergic release inhibitorsBethanidine • Bretylium • Debrisoquine • Guanadrel • Guanazodine • Guanethidine • Guanoclor • Guanoxan • Guanazodine • Guanoxabenz • GuanoxanImidazoline receptor agonistMecamylamine • Pentolinium • TrimethaphanPeripheralIndirectTyrosine hydroxylase inhibitorDirectNon-selective α blockerOther antagonists Endothelin antagonist (for PH)Ophthalmologicals: antiglaucoma preparations and miotics (S01E) Sympathomimetics Parasympathomimetics muscarinicmuscarinic/nicotinicCarbonic anhydrase inhibitors/
(sulfonamides)Beta blocking agents Prostaglandin analogues (F2α) Other agents M: EYE
anat(g/a/p)/phys/devp/prot
noco/cong/tumr, epon
proc, drug(S1A/1E/1F/1L)
Adrenergics Receptor ligands Agonists: 5-FNE • 6-FNE • Amidephrine • Anisodamine • Anisodine • Cirazoline • Dipivefrine • Dopamine • Ephedrine • Epinephrine (Adrenaline) • Etilefrine • Ethylnorepinephrine • Indanidine • Levonordefrin • Metaraminol • Methoxamine • Methyldopa • Midodrine • Naphazoline • Norepinephrine (Noradrenaline) • Octopamine • Oxymetazoline • Phenylephrine • Phenylpropanolamine • Pseudoephedrine • Synephrine • Tetrahydrozoline
Antagonists: Abanoquil • Adimolol • Ajmalicine • Alfuzosin • Amosulalol • Arotinolol • Atiprosin • Benoxathian • Buflomedil • Bunazosin • Carvedilol • CI-926 • Corynanthine • Dapiprazole • DL-017 • Domesticine • Doxazosin • Eugenodilol • Fenspiride • GYKI-12,743 • GYKI-16,084 • Indoramin • Ketanserin • L-765,314 • Labetalol • Mephendioxan • Metazosin • Monatepil • Moxisylyte (Thymoxamine) • Naftopidil • Nantenine • Neldazosin • Nicergoline • Niguldipine • Pelanserin • Phendioxan • Phenoxybenzamine • Phentolamine • Piperoxan • Prazosin • Quinazosin • Ritanserin • RS-97,078 • SGB-1,534 • Silodosin • SL-89.0591 • Spiperone • Talipexole • Tamsulosin • Terazosin • Tibalosin • Tiodazosin • Tipentosin • Tolazoline • Trimazosin • Upidosin • Urapidil • Zolertine
* Note that many TCAs, TeCAs, antipsychotics, ergolines, and some piperazines like buspirone, trazodone, nefazodone, etoperidone, and mepiprazole all antagonize α1-adrenergic receptors as well, which contributes to their side effects such as orthostatic hypotension.Agonists: (R)-3-Nitrobiphenyline • 4-NEMD • 6-FNE • Amitraz • Apraclonidine • Brimonidine • Cannabivarin • Clonidine • Detomidine • Dexmedetomidine • Dihydroergotamine • Dipivefrine • Dopamine • Ephedrine • Ergotamine • Epinephrine (Adrenaline) • Esproquin • Etilefrine • Ethylnorepinephrine • Guanabenz • Guanfacine • Guanoxabenz • Levonordefrin • Lofexidine • Medetomidine • Methyldopa • Mivazerol • Naphazoline • Norepinephrine (Noradrenaline) • Phenylpropanolamine • Piperoxan • Pseudoephedrine • Rilmenidine • Romifidine • Talipexole • Tetrahydrozoline • Tizanidine • Tolonidine • Urapidil • Xylazine • Xylometazoline
Antagonists: 1-PP • Adimolol • Aptazapine • Atipamezole • BRL-44408 • Buflomedil • Cirazoline • Efaroxan • Esmirtazapine • Fenmetozole • Fluparoxan • GYKI-12,743 • GYKI-16,084 • Idazoxan • Mianserin • Mirtazapine • MK-912 • NAN-190 • Olanzapine • Phentolamine • Phenoxybenzamine • Piperoxan • Piribedil • Rauwolscine • Rotigotine • SB-269,970 • Setiptiline • Spiroxatrine • Sunepitron • Tolazoline • Yohimbine
* Note that many atypical antipsychotics and azapirones like buspirone and gepirone (via metabolite 1-PP) antagonize α2-adrenergic receptors as well.βAgonists: 2-FNE • 5-FNE • Amibegron • Arbutamine • Arformoterol • Arotinolol • BAAM • Bambuterol • Befunolol • Bitolterol • Broxaterol • Buphenine • Carbuterol • Cimaterol • Clenbuterol • Denopamine • Deterenol • Dipivefrine • Dobutamine • Dopamine • Dopexamine • Ephedrine • Epinephrine (Adrenaline) • Etafedrine • Etilefrine • Ethylnorepinephrine • Fenoterol • Formoterol • Hexoprenaline • Higenamine • Indacaterol • Isoetarine • Isoprenaline (Isoproterenol) • Isoxsuprine • Labetalol • Levonordefrin • Levosalbutamol • Mabuterol • Methoxyphenamine • Methyldopa • Norepinephrine (Noradrenaline) • Orciprenaline • Oxyfedrine • Phenylpropanolamine • Pirbuterol • Prenalterol • Ractopamine • Procaterol • Pseudoephedrine • Reproterol • Rimiterol • Ritodrine • Salbutamol (Albuterol) • Salmeterol • Solabegron • Terbutaline • Tretoquinol • Tulobuterol • Xamoterol • Zilpaterol • Zinterol
Antagonists: Acebutolol • Adaprolol • Adimolol • Afurolol • Alprenolol • Alprenoxime • Amosulalol • Ancarolol • Arnolol • Arotinolol • Atenolol • Befunolol • Betaxolol • Bevantolol • Bisoprolol • Bopindolol • Bormetolol • Bornaprolol • Brefonalol • Bucindolol • Bucumolol • Bufetolol • Buftiralol • Bufuralol • Bunitrolol • Bunolol • Bupranolol • Burocrolol • Butaxamine • Butidrine • Butofilolol • Capsinolol • Carazolol • Carpindolol • Carteolol • Carvedilol • Celiprolol • Cetamolol • Cicloprolol • Cinamolol • Cloranolol • Cyanopindolol • Dalbraminol • Dexpropranolol • Diacetolol • Dichloroisoprenaline • Dihydroalprenolol • Dilevalol • Diprafenone • Draquinolol • Dropranolol • Ecastolol • Epanolol • Ericolol • Ersentilide • Esatenolol • Esmolol • Esprolol • Eugenodilol • Exaprolol • Falintolol • Flestolol • Flusoxolol • Hydroxycarteolol • Hydroxytertatolol • ICI-118,551 • Idropranolol • Indenolol • Indopanolol • Iodocyanopindolol • Iprocrolol • Isoxaprolol • Isamoltane • Labetalol • Landiolol • Levobetaxolol • Levobunolol • Levocicloprolol • Levomoprolol • Medroxalol • Mepindolol • Metalol • Metipranolol • Metoprolol • Moprolol • Nadolol • Nadoxolol • Nafetolol • Nebivolol • Neraminol • Nifenalol • Nipradilol • Oberadilol • Oxprenolol • Pacrinolol • Pafenolol • Pamatolol • Pargolol • Parodilol • Penbutolol • Penirolol • PhQA-33 • Pindolol • Pirepolol • Practolol • Primidolol • Procinolol • Pronethalol • Propafenone • Propranolol • Ridazolol • Ronactolol • Soquinolol • Sotalol • Spirendolol • SR 59230A • Sulfinalol • TA-2005 • Talinolol • Tazolol • Teoprolol • Tertatolol • Terthianolol • Tienoxolol • Tilisolol • Timolol • Tiprenolol • Tolamolol • Toliprolol • Tribendilol • Trigevolol • Xibenolol • XipranololReuptake inhibitors Selective norepinephrine reuptake inhibitors: Amedalin • Atomoxetine (Tomoxetine) • Ciclazindol • Daledalin • Esreboxetine • Lortalamine • Mazindol • Nisoxetine • Reboxetine • Talopram • Talsupram • Tandamine • Viloxazine; Norepinephrine-dopamine reuptake inhibitors: Amineptine • Bupropion (Amfebutamone) • Fencamine • Fencamfamine • Lefetamine • Levophacetoperane • LR-5182 • Manifaxine • Methylphenidate • Nomifensine • O-2172 • Radafaxine; Serotonin-norepinephrine reuptake inhibitors: Bicifadine • Desvenlafaxine • Duloxetine • Eclanamine • Levomilnacipran • Milnacipran • Sibutramine • Venlafaxine; Serotonin-norepinephrine-dopamine reuptake inhibitors: Brasofensine • Diclofensine • DOV-102,677 • DOV-21,947 • DOV-216,303 • JNJ-7925476 • JZ-IV-10 • Methylnaphthidate • Naphyrone • NS-2359 • PRC200-SS • SEP-225,289 • SEP-227,162 • Tesofensine; Tricyclic antidepressants: Amitriptyline • Butriptyline • Cianopramine • Clomipramine • Desipramine • Dosulepin • Doxepin • Imipramine • Lofepramine • melitracen • Nortriptyline • Protriptyline • Trimipramine; Tetracyclic antidepressants: Amoxapine • Maprotiline • Mianserin • Oxaprotiline • Setiptiline; Others: Cocaine • CP-39,332 • EXP-561 • Fezolamine • Ginkgo biloba • Indeloxazine • Nefazodone • Nefopam • Pridefrine • Tapentadol • Tedatioxetine • Teniloxazine • Tramadol • ZiprasidoneReleasing agents Morpholines: Fenbutrazate • Morazone • Phendimetrazine • Phenmetrazine; Oxazolines: 4-Methylaminorex • Aminorex • Clominorex • Cyclazodone • Fenozolone • Fluminorex • Pemoline • Thozalinone; Phenethylamines (also amphetamines, cathinones, phentermines, etc): 2-OH-PEA • 4-CAB • 4-FA • 4-FMA • 4-MA • 4-MMA • Alfetamine • Amfecloral • Amfepentorex • Amfepramone • Amphetamine (Dextroamphetamine, Levoamphetamine) • Amphetaminil • β-Me-PEA • BDB • Benzphetamine • BOH • Buphedrone • Butylone • Cathine • Cathinone • Clobenzorex • Clortermine • D-Deprenyl • Dimethylamphetamine • Dimethylcathinone (Dimethylpropion, metamfepramone) • DMA • DMMA • EBDB • Ephedrine • Ethcathinone • Ethylamphetamine • Ethylone • Famprofazone • Fenethylline • Fenproporex • Flephedrone • Fludorex • Furfenorex • Hordenine • IAP • IMP • L-Deprenyl (Selegiline) • Lisdexamfetamine • Lophophine • MBDB • MDA (Tenamfetamine) • MDEA • MDMA • MDMPEA • MDOH • MDPEA • Mefenorex • Mephedrone • Mephentermine • Methamphetamine (Dextromethamphetamine, Levomethamphetamine) • Methcathinone • Methedrone • Methylone • NAP • Ortetamine • Paredrine • pBA • pCA • Pentorex (Phenpentermine) • Phenethylamine • Pholedrine • Phenpromethamine • Phentermine • Phenylpropanolamine • pIA • Prenylamine • Propylamphetamine • Pseudoephedrine • Tiflorex • Tyramine • Xylopropamine • Zylofuramine; Piperazines: 2C-B-BZP • BZP • MBZP • mCPP • MDBZP • MeOPP • pFPP; Others: 2-Amino-1,2-dihydronaphthalene • 2-Aminoindane • 2-Aminotetralin • 2-Benzylpiperidine • 4-Benzylpiperidine • 5-IAI • Clofenciclan • Cyclopentamine • Cypenamine • Cyprodenate • Feprosidnine • Gilutensin • Heptaminol • Hexacyclonate • Indanorex • Isometheptene • Methylhexanamine • Octodrine • Phthalimidopropiophenone • Propylhexedrine (Levopropylhexedrine) • TuaminoheptaneEnzyme inhibitors 3,4-DihydroxystyreneDBHCGS-19281A • SKF-64139 • SKF-7698Nonselective: Benmoxin • Caroxazone • Echinopsidine • Furazolidone • Hydralazine • Indantadol • Iproclozide • Iproniazid • Isocarboxazid • Isoniazid • Linezolid • Mebanazine • Metfendrazine • Nialamide • Octamoxin • Paraxazone • Phenelzine • Pheniprazine • Phenoxypropazine • Pivalylbenzhydrazine • Procarbazine • Safrazine • Tranylcypromine; MAO-A selective: Amiflamine • Bazinaprine • Befloxatone • Befol • Brofaromine • Cimoxatone • Clorgiline • Esuprone • Harmala alkaloids (Harmine, Harmaline, Tetrahydroharmine, Harman, Norharman, etc) • Methylene Blue • Metralindole • Minaprine • Moclobemide • Pirlindole • Sercloremine • Tetrindole • Toloxatone • Tyrima; MAO-B selective: D-Deprenyl • Selegiline (L-Deprenyl) • Ladostigil • Lazabemide • Milacemide • Mofegiline • Pargyline • Rasagiline • Safinamide
* Note that MAO-B inhibitors also influence norepinephrine/epinephrine levels since they inhibit the breakdown of their precursor dopamine.COMTOthers Ferrous Iron (Fe2+) • S-Adenosyl-L-Methionine • Vitamin B3 (Niacin, Nicotinamide → NADPH) • Vitamin B6 (Pyridoxine, Pyridoxamine, Pyridoxal → Pyridoxal Phosphate) • Vitamin B9 (Folic acid → Tetrahydrofolic acid) • Vitamin C (Ascorbic acid) • Zinc (Zn2+)OthersActivity enhancers: BPAP • PPAP; Release blockers: Bethanidine • Bretylium • Guanadrel • Guanazodine • Guanclofine • Guanethidine • Guanoxan; Toxins: Oxidopamine (6-Hydroxydopamine)List of adrenergic drugsCategories:- Beta blockers
- Scottish inventions
Wikimedia Foundation. 2010.