- Diethylstilbestrol
-
Diethylstilbestrol 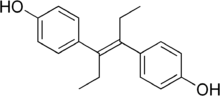
Systematic (IUPAC) name 4,4'-(3E)-hex-3-ene-3,4-diyldiphenol Clinical data AHFS/Drugs.com Micromedex Detailed Consumer Information Pregnancy cat. X Legal status ? Routes IV, oral Identifiers CAS number 56-53-1 
ATC code G03CB02 G03CC05, L02AA01 PubChem CID 448537 DrugBank DB00255 ChemSpider 395306 
UNII 731DCA35BT 
KEGG D00577 
ChEBI CHEBI:41922 
ChEMBL CHEMBL411 
Chemical data Formula C18H20O2 Mol. mass 268.35 g/mol SMILES eMolecules & PubChem  (what is this?) (verify)
(what is this?) (verify)Diethylstilbestrol (DES, former BAN stilboestrol) is a synthetic nonsteroidal estrogen that was first synthesized in 1938. Human exposure to DES occurred through diverse sources, such as dietary ingestion from supplemented cattle feed and medical treatment for certain conditions, including breast and prostate cancers. From about 1940 to 1970, DES was given to pregnant women in the mistaken belief it would reduce the risk of pregnancy complications and losses. In 1971, DES was shown to cause a rare vaginal tumor in girls and women who had been exposed to this drug in utero. The United States Food and Drug Administration subsequently withdrew DES from use in pregnant women. Follow-up studies have indicated that DES also has the potential to cause a variety of significant adverse medical complications during the lifetime of those exposed.[1] The United States National Cancer Institute recommends[2] that women born to mothers who took DES undergo special medical exams on a regular basis to screen for complications as a result of the drug. Individuals who were exposed to DES during their mothers' pregnancies are commonly referred to as "DES daughters" and "DES sons".
Contents
Synthesis
DES was first synthesized in early 1938 by Leon Golberg, then a graduate student of Sir Robert Robinson at the Dyson Perrins Laboratory at the University of Oxford, based on a formulation of Wilfrid Lawson at the Courtand Institute of Biochemistry, led by Sir Edward Charles Dodds at Middlesex Hospital Medical School of the University College London of the University of London, and a report of its synthesis was published in Nature on February 5, 1938.[3][4][5]
DES was first synthesized by English university research funded by the MRC who had a policy against patenting drugs discovered using public funds.
Clinical use
DES (in tablets up to 5 mg) was approved by the United States Food and Drug Administration on September 19, 1941 for four indications: gonorrheal vaginitis, atrophic vaginitis, menopausal symptoms, and postpartum lactation suppression to prevent breast engorgement.[5] The gonorrheal vaginitis indication was dropped when the antibiotic penicillin became available. From its very inception, the drug was highly controversial.[6][7]
In 1941, Charles Huggins and Clarence Hodges at the University of Chicago found DES to be the first effective drug for treatment of metastatic prostate cancer.[8][9] Orchiectomy or DES or both were the standard initial treatment for symptomatic advanced prostate cancer for over forty years, until the GnRH agonist leuprolide was found to have efficacy similar to DES without estrogenic effects and was approved in 1985.[10]
From the 1940s until the late 1980s, DES was FDA-approved as estrogen-replacement therapy for estrogen deficiency states such as ovarian dysgenesis, premature ovarian failure, and post-oophorectomy.
In the 1940s, DES was used off-label to prevent adverse pregnancy outcomes in women with a history of miscarriage. On July 1, 1947, the FDA approved the use of DES for this indication. The first such approval was granted to Bristol-Meyers Squibb, allowing use of 25 mg (and later 100 mg) tablets of DES during pregnancy. Approvals were granted to other pharmaceutical companies later in the same year.[11] The recommended regimen started at 5 mg per day in the 7th and 8th week of pregnancy (from first day of last menstrual period), increased every other week by 5 mg per day through the 14th week, and then increased every week by 5 mg per day from 25 mg per day in the 15th week to 125 mg per day in the 35th week of pregnancy.[12] DES was originally considered effective and safe for both the pregnant woman and the developing baby. It was aggressively marketed and routinely prescribed. Sales peaked in 1953.
In the early 1950s, a double-blind clinical trial at the University of Chicago assessed pregnancy outcomes in women who were assigned to either receive or not receive DES.[13] The study showed no benefit of taking DES during pregnancy; adverse pregnancy outcomes were not reduced in the women who were given DES. By the late 1960s, six of seven leading textbooks of obstetrics said DES was ineffective at preventing miscarriage.[11][14]
Despite an absence of evidence supporting the use of DES to prevent adverse pregnancy outcomes, DES continued to be given to pregnant women through the 1960s. In 1971, a report published in the New England Journal of Medicine showed a probable link between DES and vaginal clear cell adenocarcinoma in girls and young women who had been exposed to this drug in utero. Later in the same year, the FDA sent an FDA Drug Bulletin to all U.S. physicians advising against the use of DES in pregnant women. The FDA also removed prevention of miscarriage as an indication for DES use and added pregnancy as a contraindication for DES use.[15] On February 5, 1975, the FDA ordered 25 mg and 100 mg tablets of DES withdrawn, effective February 18, 1975.[16] The number of persons exposed to DES during pregnancy or in utero during 1940-1971 is unknown but may be as high as 2 million in the United States. DES was also used in other countries, most notably France, the Netherlands, and Great Britain.
From the 1950s through the beginning of the 1970s, DES was prescribed to prepubescent girls to begin puberty and thus stop growth by closing growth plates in the bones. Despite its clear link to cancer, doctors continued to recommend the hormone for "excess height."[17]
In 1960, DES was found to be more effective than androgens in the treatment of advanced breast cancer in postmenopausal women.[18] DES was the hormonal treatment of choice for advanced breast cancer in postmenopausal women until 1977, when the FDA approved tamoxifen, a selective estrogen receptor modulator with efficacy similar to DES but fewer side effects.[19]
In 1973, in an attempt to restrict off-label use of DES as a postcoital contraceptive (which had become prevalent at many university health services following publication of an influential study in 1971 in JAMA) to emergency situations such as rape, an FDA Drug Bulletin was sent to all U.S. physicians and pharmacists that said the FDA had approved, under restricted conditions, postcoital contraceptive use of DES.[20] In 1975, the FDA said it had not actually given (and never did give) approval to any manufacturer to market DES as a postcoital contraceptive, but would approve that indication for emergency situations such as rape or incest if a manufacturer provided patient labeling and special packaging as set out in a FDA final rule published in 1975.[21] To discourage off-label use of DES as a postcoital contraceptive, the FDA in 1975 removed DES 25 mg tablets from the market and ordered the labeling of lower doses (5 mg and lower) of DES still approved for other indications changed to state: "This drug product should not be used as a postcoital contraceptive" in block capital letters on the first line of the physician prescribing information package insert and in a prominent and conspicuous location of the container and carton label.[16][22] In the 1980s, off-label use of the Yuzpe regimen of certain regular combined oral contraceptive pills superseded off-label use of DES as a postcoital contraceptive.[23]
In 1978, the FDA removed postpartum lactation suppression to prevent breast engorgement from their approved indications for DES and other estrogens.[24] In the 1990s, the only approved indications for DES were treatment of advanced prostate cancer and treatment of advanced breast cancer in postmenopausal women. The last remaining U.S. manufacturer of DES, Eli Lilly, stopped making and marketing DES in 1997.
Associated health problems
First generation
Women who were prescribed DES during pregnancy have been shown to have a modestly increased risk of breast cancer and breast cancer mortality.
Second generation
DES daughters
DES gained notoriety when it was shown to cause a rare vaginal tumor in girls and young women who had been exposed to this drug in utero. In 1971, the New England Journal of Medicine published a report showing that 7 of 8 girls and young women (ages 14 to 22) who had been diagnosed with vaginal clear cell adenocarcinoma had been exposed prenatally to DES.[25] Subsequent studies have shown an approximate 40-fold increased risk of vaginal/cervical clear cell adenocarcinoma in women exposed in utero to DES. As a consequence of this evidence, DES is considered an established human carcinogen. DES is the only transplacental carcinogen known in humans. Daughters exposed to DES in utero may also have an increased risk of moderate/severe cervical squamous cell dysplasia and an increased risk of breast cancer.
In addition to its carcinogenic properties, DES is a known teratogen, an agent capable of causing malformations in daughters and sons who were exposed in utero. DES-exposed daughters are at an increased risk of abnormalities of the reproductive tract, including vaginal epithelial changes, an increased cervical transformation zone, and uterine abnormalities such as T-shaped uterus. These anomalies contribute to an increased risk of infertility and adverse pregnancy outcomes in prenatally DES-exposed daughters. Daughters with prenatal exposure to DES may also have an increased risk of uterine fibroids, and incompetent cervix in adulthood.[26]
In utero exposure to DES has been suggested to increase the likelihood of a girl being homosexual or bisexual.[27]
Studies have not established a link between in utero exposure to DES and autoimmune diseases.[citation needed]
DES sons
Initially, there were fewer studies documenting risks of prenatal exposure to diethylstilbestrol on males. Primarily in the 1970s and early 1980s, studies published on prenatally-DES exposed males investigated issues of increased risk of cancer, infertility and genital abnormalities in development such as cryptorchidism and hypospadias. The American Association of Clinical Endocrinologists has also formally recognized prenatal DES exposure in males as a primary risk factor associated with hypogonadism, a condition primarily associated with testosterone deficiency.[28]
The CDC does state that there is a positive correlation between diethylstilbestrol exposure and non-cancerous epididymal cysts,[29] and that exposed men are more likely to be left-handed than unexposed men.[30] Recent research on DES sons has explored the possibility that some of the effects of prenatal exposure to DES might be in the area of behavioral and or neurological change. In particular, Dr. Scott Kerlin of the DES Sons International Research Network has documented for the past 15 years "the high prevalence of individuals with confirmed or strongly suspected prenatal DES exposure who self-identify as male-to-female transsexual or transgender, and individuals who have reported experiencing difficulties with gender dysphoria."[31][32]
Various neurological changes occur after prenatal exposure of embryonic males to DES and other estrogenic endocrine disrupters. Animals that exhibited these structural neurological changes were also shown to demonstrate various gender-related behavioral changes (so called "feminisation of males"). Several published studies in the medical literature on psycho-neuro-endocrinology have examined the hypothesis that prenatal exposure to estrogens (including DES) may cause significant developmental impact on sexual differentiation of the brain, and on subsequent behavioral and gender identity development in exposed males and females.[33][34] There is significant evidence linking prenatal hormonal influences on gender identity and transsexual development.[35][36]
Psychological Anomalies
Most of the initial research documenting the psychological effects of prenatal DES exposure was poorly conducted, often by mail card. Despite that, some more carefully conducted studies show a clear link to depression[37] and lower visual-spatial reasoning skills.[38]
What has become more clear in recent years is the psychological disturbances caused by excessive prenatal estrogen exposure (regardless of source) as measured by the digit ratio. Excessive in-utero estrogen exposure may have an impact on hemispheric brain specialization, and hinder connections to the prefrontal cortex (usually associated with impulse control and concentration).[39] While exposure to DES might not specifically cause them, it may exacerbate a predisposition in individuals susceptible to schizophrenia,[40] anxiety disorders,[41] anorexia,[42] psychopathy,[43] paraphilic (or fetish) sexual interest,[44]and other neurological issues.[45]
Research into the links between excessive prenatal estrogen exposure, gender identity and resultant psychiatric conditions continues and professional opinions remain divided at this time.[46][47]
Lawsuits
In the 1970s, the negative publicity surrounding the discovery of DES's long-term effects resulted in a huge wave of lawsuits in the United States against its manufacturers. These culminated in a landmark 1980 decision of the Supreme Court of California, Sindell v. Abbott Laboratories, in which the court imposed a rebuttable presumption of market share liability upon all DES manufacturers, proportional to their share of the market at the time the drug was consumed by the mother of a particular plaintiff.
Researchers are still following the health of persons exposed to DES to determine whether other health problems occur as they grow older.
Third generation
Current research also looks at DES in the third generation. These are the children of men and women who were exposed to DES in utero; thus, they are also the grandchildren of women who were given DES during pregnancy. Studies of the third generation are important because DES might be associated with epigenetic changes. Epigenetic changes involve changes to the way genes behave (not involving the DNA itself) that may be heritable from one generation to another. If epigenetic changes occur and are heritable, studies of the DES-exposed third generation have implications for the influence of environmental endocrine disruptors on human health and evolution.
Recent results from the US National Cancer Institute (NCI) multi-center study of DES show that the daughters of DES prenatally exposed women may be less likely than the unexposed to have regular menstrual periods. A possible increased risk of infertility in the older third generation daughters was also noted. The NCI study provides limited evidence of an increased risk of birth defects in the sons or daughters of women who were exposed prenatally to DES. An increased risk of ovarian cancer in the daughters of prenatally exposed women was seen, but it was based on three cases, so the finding is considered preliminary and requires confirmation.
Some evidence suggests that the sons of prenatally DES-exposed women might have an increased risk of hypospadias[48] but other studies suggest a lower risk.[49] A possible link with hypospadias in third generation sons was suggestive but inconclusive in the NCI study, which is the only study in which the mothers' prenatal DES exposure (or lack of exposure) is verified by the medical record.
DES for canines
DES has been very successful in treating female canine incontinence stemming from poor sphincter control. It is still available from compounding pharmacies, and at the low (1 mg) dose, does not have the carcinogenic properties that were so problematic in humans. It is generally administered once a day for five days and then once every 4 to 7 days as needed.
DES in food production
During the 1960s, DES was used as a growth hormone in the beef and poultry industry. It was later found to cause cancer and was "phased out in the late 1970s."[50] Its alleged continued illegal use in the beef industry is depicted in the novel My Year of Meats, by Ruth L. Ozeki.When it was discovered that DES was harmful to humans, it was moved to veterinarian use. DES was found to cause liver failure in cats.[citation needed]
Chemistry
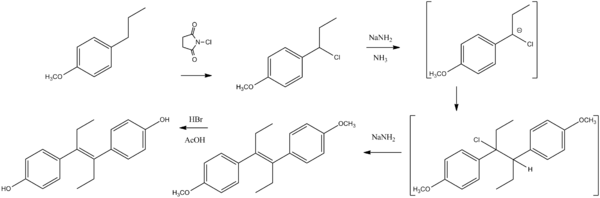 Synthesis of diethylstilbesterol.[51]
Synthesis of diethylstilbesterol.[51]
See also
- Risk factors for breast cancer
- Vaginal cancer
- National Cancer Institute DES information
- Centers For Disease Control DES patient information
References
- ^ "DES Update: For Consumers". United States Department of Health and Human Services: Centers for Disease Control and Prevention. http://www.cdc.gov/des/consumers/index.html. Retrieved 2011-06-30.
- ^ "DES: Questions and Answers". FactSheet. National Cancer Institute. http://www.cancer.gov/cancertopics/factsheet/Risk/DES. Retrieved 2011-06-30.
- ^ Dodds EC, Goldberg L, Lawson W, Robinson R (February 1938). "Estrogenic activity of certain synthetic compounds". Nature 141 (3562): 247–8. doi:10.1038/141247b0.
- ^ Dodds EC (1957). Biochemical contributions to endocrinology; experiments in hormonal research. Stanford: Stanford University Press. OCLC 1483899.
- ^ a b Meyers, Robert (1983). D.E.S., the bitter pill. New York: Seaview/Putnam. ISBN 0-399-31008-8.
- ^ Langston, Nancy (2010). Toxic bodies: Hormone disruptors and the legacy of DES. New Haven, CT: Yale University Press. ISBN 978-0-300-13607-4.
- ^ Seaman, Barbara (2003). The greatest experiment ever performed on women: Exploding the estrogen myth. New York: Hyperion. ISBN 978-0-786-86853-7.
- ^ Huggins C, Hodges CV (1972). "Studies on prostatic cancer. I. The effect of castration, of estrogen and androgen injection on serum phosphatases in metastatic carcinoma of the prostate". CA Cancer J Clin 22 (4): 232–40. doi:10.3322/canjclin.22.4.232. PMID 4625049.
- ^ "Prostate cancer yields to a drug". The New York Times: 29. Dec 15, 1943.
- ^ "Leuprolide versus diethylstilbestrol for metastatic prostate cancer. The Leuprolide Study Group". N. Engl. J. Med. 311 (20): 1281–6. November 1984. doi:10.1056/NEJM198411153112004. PMID 6436700.
- ^ a b Dutton, Diana B. (1988). Worse than the disease: pitfalls of medical progress. Cambridge: Cambridge University Press. ISBN 0-521-34023-3.
- ^ Physicians' desk reference to pharmaceutical specialties and biologicals (15th ed.). Oradell NJ: Medical Economics. 1961. p. 625. ISBN 000093447X.
- ^ Dieckmann WJ, Davis ME, Rynkiewicz LM, Pottinger RE (November 1953). "Does the administration of diethylstilbestrol during pregnancy have therapeutic value?". Am. J. Obstet. Gynecol. 66 (5): 1062–81. PMID 13104505.
- ^ Apfel R J, Fisher SM (1984). To do no harm: DES and the dilemmas of modern medicine. New Haven: Yale University Press. ISBN 0-300-03192-0.
- ^ FDA (1971). "Certain estrogens for oral or parenteral use. Drugs for human use; drug efficacy study implementation". Fed Regist 36 (217): 21537–8.; 36 F.R. 21537
- ^ a b FDA (1975). "Certain estrogens for oral use. Notice of withdrawal of approval of new drug applications". Fed Regist 40 (25): 5384.; 25 F.R. 5384
- ^ Zuger A (2009-07-27), "At What Height, Happiness? A Medical Tale", The New York Times, http://www.nytimes.com/2009/07/28/health/28book.html?ref=science
- ^ Council on Drugs (1960). "Androgens and estrogens in the treatment of disseminated mammary carcinoma: retrospective study of nine hundred forty-four patients". JAMA 172 (12): 1271–83. doi:10.1001/jama.1960.03020120049010.
- ^ Ingle JN, Ahmann DL, Green SJ, Edmonson JH, Bisel HF, Kvols LK, Nichols WC, Creagan ET, Hahn RG, Rubin J, Frytak S (January 1981). "Randomized clinical trial of diethylstilbestrol versus tamoxifen in postmenopausal women with advanced breast cancer". N. Engl. J. Med. 304 (1): 16–21. doi:10.1056/NEJM198101013040104. PMID 7001242.
- ^ Kuchera LK (October 1971). "Postcoital contraception with diethylstilbestrol". JAMA 218 (4): 562–3. doi:10.1001/jama.218.4.562. PMID 5171004.
- ^ FDA (1975). "Diethylstilbestrol as posticoital oral contraceptive; patient labeling". Fed Regist 40 (25): 5451–5.; 40 F.R. 5451
- ^ FDA (1975). "Estrogens for oral or parenteral use. Drugs for human use; drug efficacy study; amended notice". Fed Regist 40 (39): 8242.; 39 F.R. 8242
- ^ Hatcher RA, Stewart GK, Stewart F, Guest F, Josephs N, Dale J (1982). Contraceptive Technology 1982-1983. New York: Irvington Publishers. pp. 152–7. ISBN 0-829-00705-9.
- ^ FDA (1978). "Estrogens for postpartum breast engorgement". Fed Regist 43 (206): 49564–7.; 43 F.R. 49564
- ^ Herbst AL, Ulfelder H, Poskanzer DC (April 1971). "Adenocarcinoma of the vagina. Association of maternal stilbestrol therapy with tumor appearance in young women". N. Engl. J. Med. 284 (15): 878–81. doi:10.1056/NEJM197104222841604. PMID 5549830.
- ^ Office of Research on Women’s Health, NIH, DHHS (2006-03). "Status of Research on Uterine Fibroids (leiomyomata uteri) at the National Institutes of Health". United States National Institutes of Health. http://orwh.od.nih.gov/health/fibroidsrevisedmarch2006.pdf.
- ^ Ehrhardt AA, Meyer-Bahlburg HF, Rosen LR, Feldman JF, Veridiano NP, Zimmerman I, McEwen BS (February 1985). "Sexual orientation after prenatal exposure to exogenous estrogen". Arch Sex Behav 14 (1): 57–77. doi:10.1007/BF0154135. PMID 3977584.
- ^ Petak SM, Nankin HR, Spark RF, Swerdloff RS, Rodriguez-Rigau LJ (2002). "American Association of Clinical Endocrinologists Medical Guidelines for clinical practice for the evaluation and treatment of hypogonadism in adult male patients--2002 update". Endocr Pract 8 (6): 440–56. PMID 15260010. https://www.aace.com/sites/default/files/hypogonadism.pdf.
- ^ "Known Health Effects for DES Sons". United States Department of Health and Human Services: Centers for Disease Control and Prevention accessdate = 2011-06-30. http://www.cdc.gov/des/consumers/about/effects_sons.html.
- ^ Titus-Ernstoff et al (2003). "Psychosexual Characteristics of Men and Women Exposed Prenatally to Diethylstilbestrol". http://www.cdc.gov/des/consumers/research/recent_psychosexual.html.
- ^ Kerlin SP (2006-08). "Prenatal Exposure to Diethylstilbestrol (DES) in Males and Gender-related Disorders: Results from a 5-Year Study". International Behavioral Development Symposium 2005. Archived from the original on May 29, 2006. http://web.archive.org/web/20060529201743/http://www.desexposed.org/aboutdes/dessons5yrstudy.html.
- ^ Hood, E (2005-10). Are EDCs blurring issues of gender?. Environmental Health Perspectives, Vol. 113. pp. 670–677. http://ehponline.org.
- ^ Reinisch JM, Ziemba-Davis M, Sanders SA (1991). "Hormonal contributions to sexually dimorphic behavioral development in humans". Psychoneuroendocrinology 16 (1-3): 213–78. doi:10.1016/0306-4530(91)90080-D. PMID 1961841.
- ^ Yalom ID, Green R, Fisk N (April 1973). "Prenatal exposure to female hormones. Effect on psychosexual development in boys". Arch. Gen. Psychiatry 28 (4): 554–61. PMID 4734959.
- ^ Michel A, Mormont C, Legros JJ (October 2001). "A psycho-endocrinological overview of transsexualism". Eur. J. Endocrinol. 145 (4): 365–76. doi:10.1530/eje.0.1450365. PMID 11580991.
- ^ Dingfelder S (2004). "Gender Bender: New Research Suggests Genes and Prenatal Hormones Could Have More Sway in Gender Identity than Previously Thought". APA Monitor on Psychology 35(4): 48. http://www.apa.org/monitor/apr04/gender.aspx.
- ^ Pillard RC, Rosen LR, Meyer-Bahlburg H, Weinrich JD, Feldman JF, Gruen R, Ehrhardt AA (1993). "Psychopathology and social functioning in men prenatally exposed to diethylstilbestrol (DES)". Psychosom Med 55 (6): 485–91. PMID 8310108. http://www.psychosomaticmedicine.org/content/55/6/485.full.pdf.
- ^ Reinisch JM, Sanders SA (March 1992). "Effects of prenatal exposure to diethylstilbestrol (DES) on hemispheric laterality and spatial ability in human males". Horm Behav 26 (1): 62–75. PMID 1563729.
- ^ "Prenatal Testosteron makes a Genius?". The World of Science and Technology. http://www.sciencentechnologyupdates.com/2011/03/extra-prenatal-testosterone-makes.html.
- ^ Arató M, Frecska E, Beck C, An M, Kiss H (January 2004). "Digit length pattern in schizophrenia suggests disturbed prenatal hemispheric lateralization". Prog. Neuropsychopharmacol. Biol. Psychiatry 28 (1): 191–4. doi:10.1016/j.pnpbp.2003.09.020. PMID 14687873.
- ^ Kebir O, Krebs MO (March 2011). "Diethylstilbestrol and risk of psychiatric disorders: A critical review and new insights". World J Biol Psychiatry. doi:10.3109/15622975.2011.560280. PMID 21428730.
- ^ Gellene D (December 4, 2007). "Prenatal estrogen increases risk of anorexia, study finds". Los Angeles Times. http://articles.latimes.com/2007/dec/04/science/sci-anorexia4.
- ^ Blanchard, A.; Lyons, M. (2010). "An investigation into the relationship between digit length ratio (2D: 4D) and psychopathy". The British Journal of Forensic Practice 12 (2): 23. doi:10.5042/bjfp.2010.0183.
- ^ Rahman & Symeonides, Q; Symeonides, DJ (2008). "Neurodevelopmental correlates of paraphilic sexual interests in men". Archives of Sexual Behavior 37 (1): 166–172. doi:10.1007/s10508-007-9255-3. PMID 18074220. http://www.ncbi.nlm.nih.gov/pubmed/18074220.
- ^ Ferguson SA (2002). "Effects on brain and behavior caused by developmental exposure to endocrine disrupters with estrogenic effects". Neurotoxicol Teratol 24 (1): 1–3. doi:10.1016/S0892-0362(01)00196-9. PMID 11836066.
- ^ Rudacille, Deborah (1995). The Riddle of Gender: Science, Activism, and Transgender Rights. New York: Pantheon Books. ISBN 0-375-42162-9.
- ^ Meyer-Bahlburg HF (April 2010). "From mental disorder to iatrogenic hypogonadism: dilemmas in conceptualizing gender identity variants as psychiatric conditions". Arch Sex Behav 39 (2): 461–76. doi:10.1007/s10508-009-9532-4. PMC 2844928. PMID 19851856. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2844928.
- ^ Klip H, Verloop J, van Gool JD, Koster ME, Burger CW, van Leeuwen FE (March 2002). "Hypospadias in sons of women exposed to diethylstilbestrol in utero: a cohort study". Lancet 359 (9312): 1102–7. doi:10.1016/S0140-6736(02)08152-7. PMID 11943257.
- ^ Brouwers, MM.; WF. Feitz et al. (March 2006). "Hypospadias: a transgenerational effect of diethylstilbestrol?". Hum. Reprod. 21 (3): 666–669. doi:10.1093/humrep/dei398. PMID 16293648.
- ^ Gandhi R, Snedeker S (2000-06-01). "Consumer Concerns About Hormones in Food". Fact Sheet #37, June 2000. Program on Breast Cancer and Environmental Risk Factors, Cornell University. http://envirocancer.cornell.edu/factsheet/diet/fs37.hormones.cfm. Retrieved 2011-07-20.
- ^ Kharasch SM, Kleiman M (1943). J. Am. Chem. Soc. 65 (1): 11–15. doi:10.1021/ja01241a004.
External links
- DES Action USA consumer organization, providing limited information and resources for DES-exposed persons
- DES Sons International Network online research network of DES Sons
- DES Update from the U.S. Centers for Disease Control and Prevention
- DES Booklets from the U.S. National Institutes of Health (circa 1980)
- DES Follow-up Study longterm cohort study of DES-exposed persons (including the DES-AD Project)
- DES Cancer Network offers support for DES cancer victims and their families
- National Cancer Institutes's Cancer Information Service
- University of Chicago DES Registry of patients with CCA (clear cell adenocarcinoma) of the vagina and/or cervix.
Other resources
Estrogens and progestogens (G03C-D, L02) Progestogens/
progestins
(progesterone)AgonistAndrostene (Drospirenone) • 19-norprogesterone (Nomegestrol • Promegestone • Trimegestone) • 19-nortestosterone (Dienogest)Other/
ungroupedPregnenedione (Gestonorone) • Pregnene (Ethisterone) • Pregnadiene (Medrogestone • Melengestrol) • Norpregnane (Norgestrienone) • Lynestrenol • Norethynodrel • Tibolone • Dydrogesterone • Quingestanolantagonist: MifepristoneAsoprisnil • CDB-4124 • Ulipristal acetateEstrogens AgonistDiosgenin • Estradiol (Ethinylestradiol#/Mestranol • Estradiol 17 beta-cypionate# • Polyestradiol phosphate) • Estrone (Estrone sulfate) • Estriol • Promestriene • Equilenin • EquilinAfimoxifene • Arzoxifene • Bazedoxifene • Cyclofenil • Lasofoxifene • Ormeloxifene • Raloxifene • Tamoxifen • Toremifenepure antagonist: Fulvestrant#WHO-EM. ‡Withdrawn from market. Clinical trials: †Phase III. §Never to phase III Categories:- Synthetic estrogens
- Teratogens
- Withdrawn drugs
- Synthetic phenolic drugs
- IARC Group 1 carcinogens
- Eli Lilly and Company
Wikimedia Foundation. 2010.
