- Chronic inflammatory demyelinating polyneuropathy
-
For the acute version of this disease, see Guillain–Barré syndrome.
Chronic inflammatory demyelinating polyneuropathy Classification and external resources ICD-9 357.81 OMIM 139393 DiseasesDB 30084 eMedicine neuro/467 MeSH D020277 Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired immune-mediated inflammatory disorder of the peripheral nervous system. The disorder is sometimes called chronic relapsing polyneuropathy. CIDP is closely related to Guillain-Barré syndrome and it is considered the chronic counterpart of that acute disease. Its symptoms are also similar to progressive inflammatory neuropathy. An asymmetrical variant of CIDP is known as Lewis-Sumner syndrome.[1]
Contents
Overview
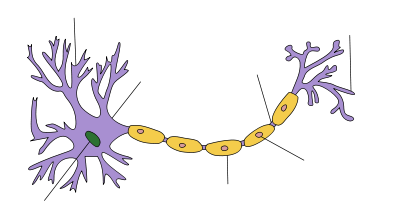
Structure of a typical neuron Neuron The pathologic hallmark of the disease is loss of the myelin sheath (the fatty covering that insulates and protects nerve fibers) of the peripheral nerves.
Chronic inflammatory demyelinating polyneuropathy is believed to be due to immune cells, cells which normally protect the body from foreign infection, but here begin incorrectly attacking the nerves in the body instead. As a result, the affected nerves fail to respond, or respond only weakly, to stimuli causing numbing, tingling, pain, progressive muscle weakness, loss of deep tendon reflexes (areflexia), fatigue, and abnormal sensations. The likelihood of progression of the disease is high.
CIDP is under-recognized and under-treated due to its heterogeneous presentation (both clinical and electrophysiological) and the limitations of clinical, serologic, and electrophysiologic diagnostic criteria. Despite these limitations, early diagnosis and treatment is important in preventing irreversible axonal loss and improving functional recovery.[2]
Lack of awareness and treatment of CIDP is also due to limitations of clinical trials. Although there are stringent research criteria for selecting patients to clinical trials, there are no generally agreed-on clinical diagnostic criteria for CIDP due to its different presentations in symptoms and objective data. Application of the present research criteria to routine clinical practice often miss the diagnosis in a majority of patients, and patients are often left untreated despite progression of their disease.[3]
In some cases electrophysiological studies fail to show any evidence of demyelination. Though conventional electrophysiological diagnostic criteria are not met, the patient may still respond to immunomodulatory treatments. In such cases, presence of clinical characteristics suggestive of CIDP are critical, justifying full investigations, including sural nerve biopsy.[4]
Diagnosis
Diagnosis is usually made through a clinical neurological examination. Patients usually present with a history of weakness, numbness, tingling, pain and difficulty in walking. They may additionally present with fainting spells while standing up or burning pain in extremities. Some patients may have sudden onset of back pain or neck pain radiating down the extremities, usually diagnosed as radicular pain. These symptoms are usually progressive and may be intermittent.
On examination the patients may have weakness, and loss of deep tendon reflexes (rarely increased or normal). There may be atrophy (shrinkage) of muscles, fasciculations (twitching) and loss of sensation. Patients may have Multi-Focal Motor neuropathy, as they have no sensory loss.
The patient may present with a single cranial nerve or peripheral nerve dysfunction.
Autonomic system dysfunction can occur; in such a case, the patient would complain of orthostatic dizziness, problems with bowel and bladder functions, and cardiac problems.
Most experts consider the necessary duration of symptoms to be greater than 8 weeks for the diagnosis of CIDP to be made.
- Electrodiagnostics - electromyography (EMG) and nerve conduction study (NCS).
In usual CIDP, the nerve conduction studies show demyelination. These findings include:
- a reduction in nerve conduction velocities b;
- the presence of conduction block or abnormal temporal dispersion in at least one motor nerve;
- prolonged distal latencies in at least two nerves;
- absent F waves or prolonged minimum F wave latencies in at least two motor nerves. (In some case EMG/NCV can be normal).
- Serum test to exclude other autoimmune diseases.
- Spinal tap and serum test for Anti-ganglioside antibodies, which are one branch of the CIDP diseases, as anti-GM1 anti-GD1a anti-GQ1b.
- Sural nerve biopsy
Biopsy is considered for those patients in whom the diagnosis is not completely clear, when other causes of neuropathy (e.g., hereditary, vasculitic) cannot be excluded, or when profound axonal involvement is observed on EMG.
Treatment
First-line treatment for CIDP includes corticosteroids (e.g. prednisone), plasmapheresis (plasma exchange) and intravenous immunoglobulin (IVIG) which may be prescribed alone or in combination with an immunosuppressant drug.[5]
IVIG and plasmapheresis have proven benefit in randomized, double-blind, placebo-controlled trials. Despite less definitive published evidence of efficacy, corticosteroids are considered standard therapies because of their long history of use and cost effectiveness. IVIG is probably the first-line CIDP treatment, but is extremely expensive (in the U.S., a single 65 g dose of Gamunex brand in 2010 might be billed at the rate of $8,000, just for the immunoglobulin, not including other charges such as nurse administration). Gamunex brand IVIG is the only U.S. FDA approved treatment for CIDP, as in 2008 Talecris, the maker of Gamunex, received orphan drug status for this drug for the treatment of CIDP.
Immunosuppressive drugs are often of the cytotoxic (chemotherapy) class, including Rituximab (Rituxan) which targets B Cells, and cyclophosphamide, a drug which reduces the function of the immune system. Ciclosporin has also been used in CIDP but with less frequency as it is a newer approach.[6] Ciclosporin is thought to bind to immunocompetent lymphocytes, especially T-lymphocytes.
Non-cytotoxic immunosuppressive treatments usually include the anti-rejection transplant drugs azathioprine (Imuran) and mycophenolate mofetil (Cellcept). In the U.S., these drugs are used as "off-label" treatments for CIDP, meaning that their use here is accepted by the FDA, but that CIDP treatment is not explicitly indicated or approved in the drug literature. Before azathioprine is used, the patient should first have a blood test that ensures that azathioprine can safely be used.
Anti-thymocyte globulin (ATG), an immunosuppressive agent that selectively destroys T lymphocytes is being studied for use in CIDP. Anti-thymocyte globulin is the gamma globulin fraction of antiserum from animals that have been immunized against human thymocytes. It is a polyclonal antibody.
Although chemotherapeutic and immunosuppressive agents have shown to be effective in treating CIDP, significant evidence is lacking, mostly due to the heterogeneous nature of the disease in the patient population in addition to the lack of controlled trials.
Physical therapy may improve muscle strength, function and mobility, and minimize the shrinkage of muscles and tendons and distortions of the joints.
Prognosis
As in multiple sclerosis, another demyelinating condition, it is not possible to predict with certainty how CIDP is going to affect an individual in the future. The pattern of relapses and remissions varies greatly with each patient. A period of relapse can be very disturbing, but many patients make significant recoveries.
If diagnosed early, initiation of early treatment to prevent loss of nerve axons is recommended. However, many individuals are left with residual numbness, weakness, tremors, fatigue and other symptoms which can lead to long-term morbidity and diminished quality of life.[7]
It is important to build a good relationship with doctors, both primary care and specialist. Because of the rarity of the illness, many doctors will not have encountered it before. Each case of CIDP is different, and relapses, if they occur, may bring new symptoms and problems. Because of the variability in severity and progression of the disease, doctors will not be able to give a definite prognosis. A period of experimentation with different treatment regimes is likely to be necessary in order to discover the most appropriate treatment regimen for a given patient.
See also
- Autoimmune diseases
- Neurology
References
- ^ http://www.cidpusa.org/LEWIS%20SUMMER.dwt
- ^ Toothaker TB, Brannagan TH (2007). "Chronic inflammatory demyelinating polyneuropathies: current treatment strategies". Curr Neurol Neurosci Rep 7 (1): 63–70. doi:10.1007/s11910-007-0023-5. PMID 17217856.
- ^ Latov N (2002). "Diagnosis of CIDP". Neurology 59 (12 Suppl 6): S2–6. PMID 12499464. http://www.neurology.org/cgi/pmidlookup?view=long&pmid=12499464.
- ^ Azulay JP (2006). "[The diagnosis of chronic axonal polyneuropathy: the poorly understood chronic polyradiculoneuritides"] (in French). Rev. Neurol. (Paris) 162 (12): 1292–5. PMID 17151528. http://www.masson.fr/masson/MDOI-RN-12-2006-162-12-0035-3787-101019-200607904.
- ^ Hughes RA (2002). "Systematic reviews of treatment for inflammatory demyelinating neuropathy". Journal of Anatomy 200 (4): 331–9. doi:10.1046/j.1469-7580.2002.00041.x. PMC 1570692. PMID 12090400. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1570692.
- ^ Odaka M, Tatsumoto M, Susuki K, Hirata K, Yuki N (2005). "Intractable chronic inflammatory demyelinating polyneuropathy treated successfully with ciclosporin". J. Neurol. Neurosurg. Psychiatr. 76 (8): 1115–20. doi:10.1136/jnnp.2003.035428. PMC 1739743. PMID 16024890. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1739743.
- ^ Kissel JT (2003). "The treatment of chronic inflammatory demyelinating polyradiculoneuropathy". Semin Neurol 23 (2): 169–80. doi:10.1055/s-2003-41130. PMID 12894382.
External links
- cidp at NINDS
- CIDP information and booklets from the Guillain-Barré Syndrome Support Group (UK and Ireland)
- The Neuropathy Association
- CIDP information from the GBS/CIDP Foundation
- Specialised reference centre for rare neuropathies
Nervous system pathology, PNS, somatic (G50–G64, 350–357) Nerve, nerve root, plexus V (Trigeminal neuralgia, Anesthesia dolorosa) · VII (Facial nerve paralysis, Bell's palsy, Melkersson–Rosenthal syndrome, Parry–Romberg syndrome, Central seven) · XI (Accessory nerve disorder)Lower limbGeneralPolyneuropathies/Polyradiculoneuropathy Guillain–Barré syndrome · Chronic inflammatory demyelinating polyneuropathyOtherCategories:- Autoimmune diseases
- Neurological disorders
Wikimedia Foundation. 2010.