- Pericarditis
-
Pericarditis Classification and external resources
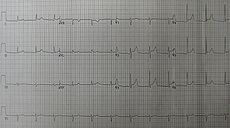
An ECG showing pericarditis. Note the ST elevation in multiple leads with slight reciprocal ST depression in aVR.ICD-10 I01.0, I09.2, I30-I32 ICD-9 420.0, 420.90, 420.91, 420.99, 423.1, 423.2 DiseasesDB 9820 MedlinePlus 000182 eMedicine med/1781 emerg/412 MeSH D010493 Pericarditis is an inflammation of the pericardium (the fibrous sac surrounding the heart). A characteristic chest pain is often present.
The causes of pericarditis are varied, including viral infections of the pericardium, idiopathic causes, uremic pericarditis, bacterial infections of the precardium (for i.e. Mycobacterium tuberculosis), post-infarct pericarditis (pericarditis due to heart attack), or Dressler's pericarditis.
Contents
Classification
Pericarditis can be classified according to the composition of the inflammatory exudate or in other words the composition of the fluid that accumulates around the heart.[1]
Types include:
- serous
- purulent
- fibrinous
- caseous
- hemorrhagic
- Post infarction
Acute vs. chronic
Depending on the time of presentation and duration, pericarditis is divided into "acute" and "chronic" forms. Acute pericarditis is more common than chronic pericarditis, and can occur as a complication of infections, immunologic conditions, or even as a result of a heart attack (myocardial infarction). Chronic pericarditis however is less common, a form of which is constrictive pericarditis. The following is the clinical classification of acute vs. chronic:
- Clinically: Acute (<6 weeks), Subacute (6 weeks to 6 months) and Chronic (>6 months)
Signs and symptoms
Substernal or left precordial pleuritic chest pain with radiation to the trapezius ridge (the bottom portion of scapula on the back), which is relieved by sitting up and bending forward and worsened by lying down (recumbent or supine position) or inspiration (taking a breath in), is the characteristic pain of pericarditis.[2] The pain may resemble the pain of angina pectoris or heart attack, but differs in that pain changes with body position, as opposed to heart attack pain that is pressure-like, and constant with radiation to the left arm and/or the jaw. Other symptoms of pericarditis may include dry cough, fever, fatigue, and anxiety. Due to similarity to myocardial infarction (heart attack) pain, pericarditis can be misdiagnosed as an acute myocardial infarction (a heart attack) solely based on the clinical data and so extreme suspicion on the part of the diagnostician is required. Ironically an acute myocardial infarction (heart attack) can also cause pericarditis, but often the presenting symptoms vary enough to warrant a diagnosis. The following table organises the clinical presentation of pericarditis:[2]
Characteristic/Parameter Pericarditis Myocardial infarction Pain description Sharp, pleuritic, retro-sternal (under the sternum) or left precordial (left chest) pain Crushing, pressure-like, heavy pain. Described as "elephant on the chest." Radiation Pain radiates to the trapezius ridge (to the lowest portion of the scapula on the back) or no radiation. Pain radiates to the jaw, or the left or arm, or does not radiate. Exertion Does not change the pain Can increase the pain Position Pain is worse supine or upon inspiration (breathing in) Not positional Onset/duration Sudden pain, that lasts for hours or sometimes days before a patient comes to the ER Sudden or chronically worsening pain that can come and go in paroxysms or it can last for hours before the patient decides to come to the ER Physical examinations
The classic sign of pericarditis is a friction rub auscultated on the cardiovascular examination usually on the lower left sternal border.[2] Other physical signs include a patient in distress, positional chest pain, diaphoresis (excessive sweating), and possibility of heart failure in form of precardial tamponade causing pulsus paradoxus, and the Beck's triad of hypotension (due to decreased cardiac output), distant (muffled) heart sounds, and JVD (jugular vein distention).
Acute complications
Pericarditis can progress to pericardial effusion and eventually cardiac tamponade. This can be seen in patients who are experiencing the classic signs of pericarditis but then show signs of relief, and progress to show signs of cardiac tamponade which include decreased alertness and lethargy, pulsus paradoxus (decrease of at least 10 mmHg of the systolic blood pressure upon inspiration), hypotension (due to decreased cardiac index), JVD (jugular vein distention from right sided heart failure and fluid overload), distant heart sounds on auscultation, and equilibration of all the diastolic blood pressures on cardiac catheterization due to the constriction of the pericardium by the fluid.
In such cases of cardiac tamponade, EKG or Holter monitor will then depict electrical alterans indicating wobbling of the heart in the fluid filled pericardium, and the capillary refill might decrease, as well as severe vascular collapse and altered mental status due to hypoperfusion of body organs by a heart that can not pump out blood effectively.
The diagnostic test for cardiac tamponade, is trans-esophageal echocardiography (TEE) although trans-thoracic echocardiography (TTE) can also be utilized in cases where there is a high suspicion of aortic dissection and high blood pressure, or in patients where esophageal probing is not feasible. Chest X-ray can depict a "water bottle" appearance of the heart in tamponade, although chest X-ray is not specific enough neither is it accurate enough in the acute setting. Of note is the fact that chest X-ray can be entirely normal in acute pericardial effusion/tamponade, so should not be relied upon as the sole diagnostic tool.
Causes
Infectious
Pericarditis may be caused by viral, bacterial, or fungal infection. The most common viral pathogen has traditionally been considered to be coxsackievirus based on studies in children from the 1960s, but recent data suggest that adults are most commonly affected with cytomegalovirus, herpesvirus, and HIV.[3][4] Pneumococcus or tuberculous pericarditis are the most common bacterial forms. Anaerobic bacteria can also be rare cause.[5] Fungal pericarditis is usually due to histoplasmosis, or in immunocompromised hosts Aspergillus, Candida, and Coccidioides. The most common worldwide cause of pericarditis is infectious pericarditis with Tuberculosis.
Other
- Idiopathic: No identifiable etiology found after routine testing.
- Immunologic conditions including systemic lupus erythematosus (more common among women) or rheumatic fever
- Myocardial Infarction (Dressler's syndrome)
- Trauma to the heart, e.g. puncture, resulting in infection or inflammation
- Uremia (uremic pericarditis)
- Malignancy (as a paraneoplastic phenomenon)
- Side effect of some medications, e.g. isoniazid, cyclosporine, hydralazine, warfarin, and heparin
- Radiation induced
- Aortic dissection
- Tetracyclines
- Postpericardiotomy syndrome: Usually after CABG surgery
Laboratory tests
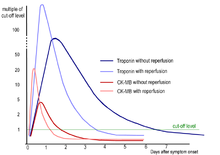
Laboratory values can show increased uric acid (BUN), or increased blood creatinine in cases of uremic pericarditis. Generally however, laboratory values are normal, but if there is a concurrent myocardial infarction (heart attack) or great stress to the heart, laboratory values may show increased cardiac markers like Troponin (I, T), CK-MB, Myoglobin, and LDH1 (Lactase Dehydrogenase isotype 1). The preferred intial diagnostic testing is the EKG which will show a 12-lead electrocardiogram with diffuse, non-specific, concave, ST segment-elevations all leads except aVR and V1[2] and PR segment-depression possible in any lead except aVR;[2] sinus tachycardia, and low-voltage QRS complexes can also be seen if there is subsymptomatic levels of pericardial effusion.
Since the mid-19th Century, retrospective diagnosis of pericarditis has been made upon the finding of adhesions of the pericardium.[6] When pericarditis is diagnosed clinically, the underlying cause is often never known; it may be discovered in only 16[7] to 22[8] percent of patients with acute pericarditis.
Treatment
The treatment in viral or idiopathic pericarditis is with Aspirin,[2] or non-steroidal anti-inflammatory drugs (NSAIDs such as naproxen). Severe cases may require:
- pericardiocentesis to treat pericardial effusion/tamponade
- antibiotics to treat tuberculosis or other bacterial causes.
- steroids are used in acute pericarditis but are not favored because they increase chance of recurrent pericarditis.
- colchicine is a very effective treatment option. If Aspirin and NSAIDs are not sufficient, colchicine should be added to the regimen.
- in rare cases, surgery
References
- ^ images
- ^ a b c d e f American College of Physicians (ACP). Medical Knowledge Self-Assessment Program (MKSAP-15): Cardiovascular Medicine. "Pericardial disease." p. 64. ISBN 978-934465-28-8 [1]
- ^ AU Corey GR; Campbell PT; Van Trigt P; Kenney RT; O'Connor CM; Sheikh KH; Kisslo JA; Wall TC (August 1993). "Etiology of large pericardial effusions". American Journal of Medicine 95 (2): 209–13. doi:10.1016/0002-9343(93)90262-N. PMID 8356985.
- ^ Campbell PT; Li JS; Wall TC; O'Connor CM; Van Trigt P; Kenney RT; Melhus O; Corey GR (April 1995). "Cytomegalovirus pericarditis: a case series and review of the literature". American Journal of Medical Science 309 (4): 229–34. doi:10.1097/00000441-199504000-00009. PMID 7900747.
- ^ Brook I. Pericarditis caused by anaerobic bacteria.Int J Antimicrob Agents 2009; 297-300.
- ^ Austin Flint (1862). "Lectures on the diagnosis of diseases of the heart: Lecture VIII". American Medical Times: Being a weekly series of the New York Journal of Medicine 5 (July to December): 309–311.
- ^ Permanyer-Miralda G; Sagrista-Sauleda J; Soler-Soler J (October 1, 1985). "Primary acute pericardial disease: a prospective series of 231 consecutive patients". American Journal of Cardiology 56 (10): 623–30. doi:10.1016/0002-9149(85)91023-9. PMID 4050698.
- ^ Zayas R; Anguita M; Torres F; Gimenez D; Bergillos F; Ruiz M; Ciudad M; Gallardo A; Valles F (February 15, 1995). "Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis". American Journal of Cardiology 75 (5): 378–82. doi:10.1016/S0002-9149(99)80558-X. PMID 7856532.
General References
- Troughton RW, Asher CR and Klein AL. Pericarditis, Lancet 2004;363:717-27. http://www.ncbi.nlm.nih.gov/pubmed/15001332
- Maisch B, Seferović PM, Ristić AD, et al. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task Force on the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology. European Heart Journal 2004;25:587-610. http://eurheartj.oxfordjournals.org/cgi/content/full/25/7/587
External links
- Pericarditis - Cleveland Clinic
- Pericarditis - National Library of Medicine
- Pericarditis - National Heart Lung Blood Institute
Inflammation Acute preformed: Lysosome granules · vasoactive amines (Histamine, Serotonin)
synthesized on demand: cytokines (IFN-γ, IL-8, TNF-α, IL-1) · eicosanoids (Leukotriene B4, Prostaglandins) · Nitric oxide · KininsChronic Processes Traditional: Rubor · Calor · Tumor · Dolor (pain) · Functio laesa
Modern: Acute-phase reaction/Fever · Vasodilation · Increased vascular permeability · Exudate · Leukocyte extravasation · ChemotaxisSpecific locations CNS (Encephalitis, Myelitis) · Meningitis (Arachnoiditis) · PNS (Neuritis) · eye (Dacryoadenitis, Scleritis, Keratitis, Choroiditis, Retinitis, Chorioretinitis, Blepharitis, Conjunctivitis, Iritis, Uveitis) · ear (Otitis, Labyrinthitis, Mastoiditis)CardiovascularCarditis (Endocarditis, Myocarditis, Pericarditis) · Vasculitis (Arteritis, Phlebitis, Capillaritis)upper (Sinusitis, Rhinitis, Pharyngitis, Laryngitis) · lower (Tracheitis, Bronchitis, Bronchiolitis, Pneumonitis, Pleuritis) · MediastinitisDigestivemouth (Stomatitis, Gingivitis, Gingivostomatitis, Glossitis, Tonsillitis, Sialadenitis/Parotitis, Cheilitis, Pulpitis, Gnathitis) · tract (Esophagitis, Gastritis, Gastroenteritis, Enteritis, Colitis, Enterocolitis, Duodenitis, Ileitis, Caecitis, Appendicitis, Proctitis) · accessory (Hepatitis, Cholangitis, Cholecystitis, Pancreatitis) · PeritonitisArthritis · Dermatomyositis · soft tissue (Myositis, Synovitis/Tenosynovitis, Bursitis, Enthesitis, Fasciitis, Capsulitis, Epicondylitis, Tendinitis, Panniculitis)
Osteochondritis: Osteitis (Spondylitis, Periostitis) · Chondritisfemale: Oophoritis · Salpingitis · Endometritis · Parametritis · Cervicitis · Vaginitis · Vulvitis · Mastitis
male: Orchitis · Epididymitis · Prostatitis · Balanitis · Balanoposthitis
pregnancy/newborn: Chorioamnionitis · OmphalitisCategories:- Pericardial disorders
- Diseases involving the fasciae
- Inflammations
Wikimedia Foundation. 2010.