- Thoracic outlet syndrome
-
Thoracic outlet syndrome Classification and external resources 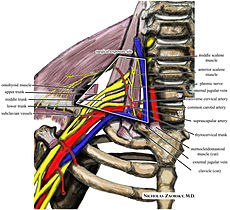
The right brachial plexus, viewed from in front. In thoracic outlet syndrome there is compression of the brachial plexus or subclavian vessels in their passage from the cervical and upper thoracic area toward the axilla and proximal arm. The anterior supraclavicular neurosurgical procedure is used to treat certain refractory cases.ICD-10 G54.0 ICD-9 353.0 DiseasesDB 13039 MedlinePlus 001434 eMedicine pmr/136 MeSH D013901 Thoracic outlet syndrome (TOS) is a syndrome involving compression at the superior thoracic outlet[1] involving compression of a neurovascular bundle passing between the anterior scalene and middle scalene.[2] It can affect the brachial plexus (nerves that pass into the arms from the neck), and/or the subclavian artery or rarely the vein which does not normally pass through the scalene hiatus (blood vessels as they pass between the chest and upper extremity). Rarely a Pancoast tumour in the apex of the lung may be the cause.
The compression may be positional (caused by movement of the clavicle (collarbone) and shoulder girdle on arm movement) or static (caused by abnormalities or enlargement or spasm of the various muscles surrounding the arteries, veins, and brachial plexus), a first rib fixation and a cervical rib.
Common orthopaedic tests used are the Adson's test, the CostoClavicular manoeuvre and the Hands-Up test of East. Careful examination and X-ray are required to differentially diagnose between positional and static aetiology, first rib fixations, scalene muscle spasm and a cervical rib or fibrous band.
Contents
Classification
By structures affected & symptomatology
There are three main types of TOS, named according to the cause of the symptoms; however these 3 classifications have been coming into disfavor because TOS can involve all 3 types of compression to various degrees: The compression occurs in three anatomical structures, arteries, veins and nerves; isolated, or more commonly two or three of the structures are compressed. Compression can be of different magnitude in each of these structures. Therefore symptoms can be protean.[3] http://www.tos-syndrome.com/old1/newpage12.htm[4]
- neurogenic TOS, disorders produced by compression of the components of the brachial plexus nerves. The neurogenic form of TOS accounts for 95% of all cases of TOS.[5]
- arterial TOS, caused by compression of the subclavian artery.[5]
- venous TOS, caused by compression of the subclavian vein.[5]
By event
There are many causes of TOS. The most frequent cause is trauma, either sudden, as in a clavicle fracture caused by a car accident, or repetitive trauma, as in a legal secretary who works with his hands, wrists, and arms at a fast paced desk station with non-ergonomic posture for many years. TOS is also found in certain occupations involving lots of lifting of the arms and repetitive use of the wrists and arms.
One cause of arterial compression is trauma, and a recent case involving fracture of the clavicle has been reported[6]
The two groups of people most likely to develop TOS are those suffering from neck injuries from traffic collisions and those who use computers in non-ergonomic postures for extended periods of time. It is a frequent repetitive stress injury caused by certain types of work environments. Other groups which may develop TOS, are athletes who frequently raise their arms above the head (such as swimmers, volleyball players, shuttle players, baseball pitchers, and weightlifters), rock climbers, electricians who work long hours with their hands above their heads and also some musicians.
By structure causing constriction
It is also possible to classify TOS by the location of the obstruction:
- Scalenus anticus syndrome (compression on brachial plexus and/or subclavian artery caused by muscle growth) – diagnosed by using Adson's sign with patient's head turned outward.
- Cervical rib syndrome (compression on brachial plexus and/or subclavian artery caused by bone growth) – diagnosed by using Adson's sign with patient's head turned inward.
- Costoclavicular syndrome (narrowing between the clavicle and the first rib) – diagnosed with the costoclavicular maneuver.
Some people are born with an extra, incomplete and very small rib above the first rib, which protrudes out into the superior thoracic outlet space and this rib causes fibrous changes around the brachial plexus nerves and causes the symptoms of Thoracic Outlet Syndrome. This is called a Cervical Rib, and is attached to the C-7. The symptoms of Thoracic Outlet Syndrome can first appear in the early teen years as a child is becoming more athletic. Surgical removal of this rib is almost always recommended.
Symptoms and consequences
TOS affects mainly the upper limbs, especially the arms and hands. Pain in the arms and hands is almost always present. Pain can be sharp, burning, or aching. Pain can involve only part of the hand, as in the 4th and 5th finger only, or all of the hand. It can involve the inner aspect of the forearm and upper arm. Pain can also be in the side of the neck, the pectoral area below the clavicle, the axillary area, and the upper back, as in the trapezius and rhomboid area. Decoloration of the hands is also a possible symptom, and one hand colder than the other hand is also common. Weakness of the hand and arm muscles is also common. Tingling can also be present.
TOS is often the underlying cause of stubborn upper limb conditions like frozen shoulder and carpal tunnel syndrome that defy standard treatment protocols.
Cerebrovascular arterial insufficiency when they affect the subclavian artery.[7] It also can affect the vertebral artery, case in which it could produce transient blindness,[8] and embolic cerebral infarction.[9]
A painful, swollen and blue arm, usually occurring after strenuous physical activity, could be a sign of a venous compression or subclavian vein thrombosis, called Paget-Schroetter Syndrome.
Diagnosis
Adson's sign and the costoclavicular maneuver are notoriously inaccurate, and may be a small part of a comprehensive history and physical examination of a patient with TOS. There is currently no single clinical sign that makes the diagnosis of TOS with certainty.
Additional maneuvers that may be abnormal are the stick em up "hand raise" for up to 3–5 minutes (holding both hands at right angles bent at the elbows over head, with or without hand opening and closing fingers, the affected hand will often quickly become paler than the unaffected because of compromised blood supply) and the "compression test" (pressure between the clavicle and medial humeral head causes radiation of pain / numbness into the affected arm).[10]
Other Radiographic & helpful Diagnostic Tools to help determine Thoracic Outlet Syndrome
Doppler Arteriography, with probes at the fingertips and arms, tests the force of the arterial flow through the radial arteries and then having the patient perform various arm maneuvers (which causes compression of the subclavian artery at the thoracic outlet) is very helpful to evaluate thoracic outlet syndrome, by eliciting symptoms of pain, numbness and graphs with diminished arterial blood flow to the fingertips with various arm maneuvers provides strong evidence of impingement of the subclavian artery at the thoracic outlet.[11]
MRI/MRA Special high resolution MRI/MRA of the Brachial Plexus
Some physicians advocate the injection of a short-acting anesthetic such as xylocaine or marcaine into the anterior scalene, subclavius, or pectoralis minor muscles as a provocative test to assist in the diagnosis of thoracic outlet syndrome. This is referred to as a 'scalene block' with the use of Lidocaine or similar drug. However, this is not considered a 'treatment', as the relief is expected to wear off within an hour or two, at a maximum. Active research continues into the accuracy and risks of this provocative test.[citation needed] Current research on TOS and the use of Blocks is underway at Johns Hopkins Hospital, Baltimore, MD.
Treatment
Most patients respond to conservative measures. Only a minority of patients with signs and symptoms of TOS ultimately proceed to surgery.
Noninvasive
The goal of self stretching is to relieve compression in the thoracic cavity, reduce blood vessel and nerve impingement, and realign the bones, muscles, ligaments, and tendons causing the problem.
- Moving shoulders forward (hunching) then back to neutral, followed by extending them back (arching) then back to neutral, followed by lifting shoulders then back to neutral.
- Tilting and extending neck opposite to the side of injury while keeping the injured arm down or wrapped around the back.
- Nerve Gliding
This syndrome causes a compression of a large cluster of nerves, resulting in the impairment of nerves throughout the arm. By performing nerve gliding exercises one can stretch and mobilize the nerve fibers. Chronic and intermittent nerve compression has been studied in animal models, and has a well-described pathophysiology, as described by Susan Mackinnon, MD, currently at Washington University in St. Louis. Nerve gliding exercises have been studied by several authorities, including David Butler in Australia.
- Extend your injured arm with fingers directly outwards to the side. Tilt your head to the otherside, and/or turn your head to the other side. A gentle pulling feeling is generally felt throughout the injured side. Initially, only do this and repeat. Once this exercise has been mastered and no extreme pain is felt, begin stretching your fingers back. Repeat with different variations, tilting your hand up, backwards, or downwards.
TOS is rapidly aggravated by poor posture. Active breathing exercises and ergonomic desk setup can both help maintain active posture. Often the muscles in the back become weak due to prolonged (years) hunching.
- Ice/Heat
Ice can be used to decrease inflammation of sore or injured muscles. Heat can also aid in relieving sore muscles by improving circulation to them. While the whole arm generally feels painful, some relief can be seen when ice/heat is applied to the thoracic region (collar bone, armpit, or shoulder blades).
Acupuncture is also an effective method of treatment for TOS. Patients may feel significantly less pain within 3-4 acupuncture treatment sessions.
Invasive
Injected into a joint or muscle, cortisone can help relief and lower inflammation.[dubious ]
- Botox injections
Botox, short for Botulinum Toxin A, binds nerve endings and prevents the release of neurotransmitters that activate muscles. A small amount of Botox injected into the tight or spastic muscles (usually one or all three scalenes) found in TOS sufferers often provides months of relief while the muscle is temporarily paralyzed. This noncosmetic treatment is unfortunately not covered by most medical plans and costs upwards of $400. The relief of symptoms from a Botox injection generally lasts 3–4 months, at which point the Botox toxin is degraded by the affected muscles. Serious side effects have been reported, and are similarly long-lasting, so improved understanding of the mechanism of a 'scalene block' is vital to determining the benefit and risk of using Botox. Additionally, many[according to whom?] patients report no relief of symptoms from Botox or scalene injections, which may indicate that the pain does not stem from the scalene muscle, and may not be TOS. Botox can be a effective treatment for neurogenic TOS.[12] It may allow for the patient to apply physical therapy pain free and thereby be able to properly stretch and open up the compressed area.
Surgical Approaches
Surgical approaches have also been used.[13] In cases where the first rib is compressing a vein, artery, or the nerve bundle, the first rib and scalene muscles and compressive fibrous tissue can be removed. The procedure is called a first rib resection and scalenectomy and involves going through the underarm area or anterior scalene neck area and removing the first rib, scalene muscles, and any compressive fibrous tissue to open the area to allow blood flow and reduce nerve compression. In some cases there is also a rudimentary rib, or a cervical rib that can be causing compression, which can be removed using the same technique.
Physical therapy is used both before the operation and after to further the patient's success in recovery. Complications include pneumothorax, infection, loss of feeling, pain, and as in all surgeries, a very small risk of death and a risk of permanent lifelong injury.
Notable patients
Major League Baseball players Matt Harrison, Hank Blalock, John Rheinecker, Jeremy Bonderman, Alex Cobb, Kenny Rogers, Jarrod Saltalamacchia, and Noah Lowry[14] have recently been diagnosed with Thoracic outlet syndrome. Kenny Rogers was diagnosed several years earlier with TOS in the other upper extremity. Coincidentally, five of these eight players have played for the Texas Rangers. All-Star pitcher J. R. Richard suffered a career-ending stroke from an undiagnosed case of TOS. Pitcher David Cone had a variant case of TOS, with an arterial aneurysm of the upper aspect of his pitching arm. Craig Carton of WFAN had Thoracic outlet syndrome and underwent successful microsurgery to cure it.
Overhead athletes, such as swimmers, track and field runners such as (Eric Baumgartner) and volleyball players, are known to be predisposed to the development of TOS.
Musician Isaac Hanson suffered a potentially life threatening pulmonary embolism as a complication of thoracic outlet syndrome.[15]
See also
- Paget-Schroetter disease
- May-Thurner syndrome - Similar compression in the left common iliac vein.
References
- ^ MeSH Thoracic+outlet+syndrome
- ^ Jay Allan Liveson (25 September 2000). Peripheral neurology: case studies. Oxford University Press US. pp. 255–. ISBN 9780195135633. http://books.google.com/books?id=nARrfwZPVH8C&pg=PA255. Retrieved 4 August 2010.
- ^ Ambrad-Chalela, Esteban; Thomas, George I.; Johansen, Kaj H. (2004). "Recurrent neurogenic thoracic outlet syndrome". The American Journal of Surgery 187 (4): 505–10. doi:10.1016/j.amjsurg.2003.12.050.
- ^ Selmonosky, M.D., Carlos. "TOS-Syndrome; Symptoms". http://www.tos-syndrome.com. Retrieved 2011-03-20.
- ^ a b c Fugate, Mark W.; Rotellini-Coltvet, Lisa; Freischlag, Julie A. (2009). "Current management of thoracic outlet syndrome". Current Treatment Options in Cardiovascular Medicine 11 (2): 176–83. doi:10.1007/s11936-009-0018-4. PMID 19289030.
- ^ Burnand, K. M.; Lagocki, S.; Lahiri, R. P.; Tang, T. Y.; Patel, A. D.; Clarke, J. M. F. (2010). "Persistent subclavian artery stenosis following surgical repair of non-union of a fractured clavicle". Grand Rounds 10: 55–8. doi:10.1102/1470-5206.2010.0012. http://www.grandrounds-e-med.com/articles/gr100012.pdf.
- ^ Thetter, O; Van Dongen, RJ; Barwegen, MG (1985). "The thoracic outlet compression syndrome and its vascular complications". Zentralblatt fur Chirurgie 110 (8): 449–56. PMID 4002908.
- ^ Sell, James J.; Rael, Jesse R.; Orrison, William W. (1994). "Rotational vertebrobasilar insufficiency as a component of thoracic outlet syndrome resulting in transient blindness". Journal of Neurosurgery 81 (4): 617–9. doi:10.3171/jns.1994.81.4.0617. PMID 7931599.
- ^ Nishibe, T; Kunihara, T; Kudo, FA; Adachi, A; Shiiya, N; Murashita, T; Matusi, Y; Yasuda, K (2000). "Arterial thoracic outlet syndrome with embolic cerebral infarction. Report of a case". Panminerva medica 42 (4): 295–7. PMID 11294095.
- ^ http://www.nismat.org/ptcor/thoracic_outlet
- ^ Thoracic outlet syndrome Mount Sinai Hospital, New York
- ^ Christo, Paul J; Dana K Christo; Adam J Carinci; Julie A Freischlag (April 2010). "Single CT-Guided Chemodenervation of the Anterior Scalene Muscle with Botulinum Toxin for Neurogenic Thoracic Outlet Syndrome". Pain Medicine 11 (4): 504–511.
- ^ Rochkind, S; Shemesh, M; Patish, H; Graif, M; Segev, Y; Salame, K; Shifrin, E; Alon, M (2007). "Thoracic outlet syndrome: a multidisciplinary problem with a perspective for microsurgical management without rib resection". Acta neurochirurgica. Supplement 100: 145–7. doi:10.1007/978-3-211-72958-8_31. PMID 17985565.
- ^ San Francisco Chronicle: Lowry's agent lashes out
- ^ "People Magazine". Archived from the original on October 18, 2007. http://web.archive.org/web/20071018005700/http://www.hanson.net/site/hanson/blog_entry/1?entry_id=5832. Retrieved 2008-01-01.
External links
- thoracic at NINDS
- Thoracic Outlet Syndrome PART I: A clinical review, Journal of American Chiropractic Association
- Physical Therapy Corner - Thoracic Outlet Syndrome
- Society for Vascular Surgery (U.S.)
- Thoracic Outlet Syndrome Patient Information
Nervous system pathology, PNS, somatic (G50–G64, 350–357) Nerve, nerve root, plexus V (Trigeminal neuralgia, Anesthesia dolorosa) · VII (Facial nerve paralysis, Bell's palsy, Melkersson–Rosenthal syndrome, Parry–Romberg syndrome, Central seven) · XI (Accessory nerve disorder)Lower limbGeneralPolyneuropathies/Polyradiculoneuropathy OtherCategories:- Peripheral nervous system disorders
- Syndromes
Wikimedia Foundation. 2010.
