- Vasectomy
-
Vasectomy 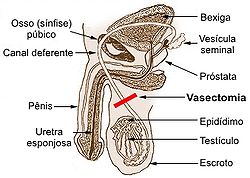
Diagram showing the usual location of a vasectomy.Background Birth control type Sterilization First use 1899 (experiments from 1785)[1] Failure rates (first year) Perfect use <0.1% Typical use 0.15%, "Vas-Clip" nearly 1% Usage Duration effect Permanent Reversibility Possible, but expensive. User reminders 2 consecutive negative semen specimens required to verify azoospermia. Clinic review All Advantages and disadvantages STD protection No Benefits No need for general anesthesia. Lower cost/less invasive than tubal ligation for women. Risks Temporary local inflammation or swelling of the testes. Long-term genital pain (PVPS). Vasectomy is a surgical procedure for male sterilization and/or permanent birth control. During the procedure, the vasa deferentia of a man are severed, and then tied/sealed in a manner such to prevent sperm from entering into the seminal stream (ejaculate). Vasectomies are usually performed in a physician's office or medical clinic.
There are several methods by which a surgeon might complete a vasectomy procedure, all of which occlude (seal) at least one side of each vas deferens. To help reduce anxiety and increase patient comfort, men who have an aversion to needles might opt for the "no-needle" application of anesthesia while the "no-scalpel" or "open-ended" techniques help to speed-up recovery times and increase the chance of healthy recovery.
Due to the simplicity of the surgery, a vasectomy usually takes less than 30 minutes to complete. After a short recovery at the doctor's office (usually less than an hour), the patient is sent home to rest. Because the procedure is minimally invasive, many vasectomy patients find that they can resume their typical lifestyle routines within a week, and do so with minimal discomfort.
Because the procedure is considered a permanent method of birth control (not easily reversed), men are usually counseled/advised to consider how the long-term outcome of a vasectomy might affect them both emotionally and physically.
-
- Misnomer:
- Vasectomy should not be confused with castration, which is the surgical removal of the testicle(s).
-
- Gender Comparison:
- The alternative/corresponding female surgical sterilization procedure known as Tubal ligation is considered major surgery usually done with general anesthesia (or with an epidural at child-birth), typically done at an in-patient, hospital setting. The prevalence of tubal ligation is higher (compared to men having vasectomies), due to the ability of a surgeon to complete this procedure in a child birth setting
Procedure
The traditional incision approach of vasectomy involves numbing of the scrotum with local anesthetic (although some men's physiology may make access to the vas deferns more difficult in which case general anesthesia is recommended) after which a scalpel is used to make two small incisions on each side of the scrotum at a location that allows the surgeon to bring each vas deferens to the surface for excision. The vasa deferentia are cut (sometimes a piece removed), separated and then at least one side is sealed by ligating (suturing), cauterizing (electrocauterization), or clamping.[2] Currently, there are several variations to this method that improve healing, effectiveness and help mitigate long-term pain such as Post-vasectomy pain syndrome (PVPS)
- No-Scalpel vasectomy: Also known as a "key-hole" vasectomy,[3] in which a sharp hemostat (as opposed to a scalpel), is used to puncture the scrotum (scrotal sac). This method has come in to widespread use as the resulting smaller "incision" or puncture wound typically limits bleeding and hematomas. Also the smaller wound has less chance of infection, resulting in faster healing times compared to the larger/longer incisions made with a scalpel. The surgical wound created by the No-Scalpel method usually does not require stitch(es).
- Open-Ended vasectomy: The testicular end of the vas deferens is not sealed, which allows continued streaming of sperm into the scrotum. This method may avoid testicular pain as a result of increased back-pressure in the epididymis.[4] Studies suggest that this method may reduce long-term complications such as Post-vasectomy pain syndrome.
- No-Needle anesthesia: Fear of needles for injection of local anesthesia is well known.[5] In 2005, a method of local anesthesia was introduced for vasectomy which allows the surgeon to apply it painlessly with a special jet-injection tool, as opposed to traditional needle application. The numbing agent is forced/pushed onto and deep enough into the scrotal tissue to allow for a virtually pain-free surgery. Initial surveys[5] show a very high satisfaction rate amongst vasectomy patients. Once the effects of no-needle anesthesia take effect, all other aspects of the vasectomy surgery remain the same.
- Fascial Interposition: Recanalization[6] of the vas deferens is a known cause of vasectomy failure(s). Fascial Interposition ("FI") helps to prevent this type of failure, increasing the overall success rate of vasectomy. FI is the positioning of the prostatic "receiving" end of the vas deferens to the outside of the fascial sheath[7] while leaving the testicular end within the confines of the fascia. The Fascia is a fibrous protective sheath that surrounds the vas deferens. This method, when combined with intraluminal cautery (one or both sides of the vas deferens), has been shown to increase the success rate of vasectomy procedures.
- Vas Irrigation: Injections of sterile water or euflavine (which kills sperm) in to the distal portion of the vas at the time of surgery brings about a near-immediate sterile (azoospermatic) condition. The use of euflavine did however, decrease time (or, number of ejaculations) to azoospermia vs. the water irrigation by itself. This additional step in the vasectomy procedure (and similarly, fascial interposition), has shown positive results but is not as prominent in use, given the fact that few surgeons offer it as part of their vasectomy procedure.[8]
Less Prominent Techniques
The following methods to vasectomy purportedly have a better chance of reversal, but have seen less use by virtue of higher failure rates and poor long term statistical information as to overall success.
- Clip: A vasectomy using a mechanical clip does not require cutting the vas deferens, but rather uses a clip to squeeze shut the flow of sperm.
An earlier clip device, the VasClip, is no longer on the market, due to unacceptably high failure rates.[9][10][11] A new clip device, the Pro-Vas, is currently available.[12]
The VasClip method had a higher cost and resulted in lower success rates. Also, because vas deferens is not cut and/or tied with this method, it may not technically be considered vasectomy. Vasectomy reversal (and the success thereof) was conjectured to be higher as it only required removing the Vas-Clip. This method appeared to only be in limited use, and therefore little reversal data is available.[11]
Vas Occlusion Techniques
- Intra-Vas Device: The vasa deferentia can also be occluded by an Intra-Vas Device or "IVD". A small cut is made after which a soft silicone or urethane plug is inserted in to each vas tube thereby blocking (occluding) sperm. This method allows for the vas to remain intact. IVD technique is done in an out-patient setting with local anesthetic, just like a traditional vasectomy. IVD reversal can be performed under the same conditions making it much less costly than vasovasostomy which usually requires general anesthesia and longer surgery time.[13]
- Injected Plugs: Similar to the Intra-Vas Device technique, there are 2 types of injected plugs. Medical-grade polyurethane (MPU) or medical-grade silicone rubber (MSR), starts as a liquid polymer that is injected in to the vas deferens after which the liquid is clamped in place until is solidifies (usually in a few minutes).[14]
Both vas occlusion techniques require the same basic patient setup hence local anesthetic, puncturing of the scrotal sac for access of the vas and then plug and/or injected plug occlusion. The success of the aforementioned vas occlusion techniques remains to be seen as there limited statistical reports as to reliability, reversal and/or use to date. Studies have shown however, that the time to achieve sterility is longer than the more prominent techniques mentioned in this text. The satisfaction rate of patients undergoing IVD techniques does however have a high rate of satisfaction as relates to the surgery experience itself.[8]
Outlook
 A post-vasectomy scrotum, showing typical post-operative bruising, incision stitches and a shaved scrotum.
A post-vasectomy scrotum, showing typical post-operative bruising, incision stitches and a shaved scrotum.
Sexual intercourse can usually be resumed in about a week (depending on recovery); however, pregnancy is still possible as long as the sperm count is above zero. Another method of birth control must be used until a follow-up sperm count test two months after the vasectomy, or after 10 to 20 ejaculations over a shorter period of time, can be performed.[citation needed]
After vasectomy contraceptive precautions have to be continued till azospermia is confirmed. Usually two semen analysis at 3 and 4 months are necessary to confirm azospermia. British Andrological Society has recommended that a single semen analysis confirming azospermia after 16 weeks is sufficient.
Biological
Vasectomy essentially ensures that the patient will be sterile after surgery. The procedure is regarded by the medical profession as permanent because vasectomy reversal is costly and often does not restore the sperm count and/or motility to pre-vasectomy levels.
Men with vasectomies have a very small (nearly zero) chance of making a woman pregnant, but they will still have exactly the same risk of contracting and spreading sexually transmitted infections. For vasectomized men who are not in monogamous relationships, the rate of acquired STD's may be higher (compared to a similar cross-section of non-vasectomized men), due to the elimination of pregnancy risk, and therefore lack of using barrier protection (condoms). In short, a man who is active with new partners would be more likely to use barrier protection if he has not had a vasectomy[citation needed].
After vasectomy, the testes remain in the scrotum where Leydig cells continue to produce testosterone and other male hormones that continue to be secreted into the blood stream. One study found that sexual desire after vasectomy was diminished in 6% of vasectomized men,[15] whereas other studies find higher rates of diminished sexual desire, for example nearly 20%.[16]
When the vasectomy is complete, sperm cannot exit the body through the penis. Sperm are still produced by the testicles, but they are broken down and absorbed by the body. Much fluid content is absorbed by membranes in the epididymis, and much solid content is broken down by the responding macrophages and re-absorbed via the blood stream. Sperm is matured in the epididymis for about a month before leaving the testicles. After vasectomy, the membranes must increase in size to absorb and store more fluid; this triggering of the immune system causes more macrophages to be recruited to break down and re-absorb more solid content. Within one year after vasectomy, sixty to seventy percent of vasectomized men develop antisperm antibodies.[17] In some cases, vasitis nodosa, a benign proliferation of the ductular epithelium, can also result.[18][19] The buildup of sperm increases pressure in the vas deferens and epididymis. The entry of the sperm into the scrotum causes sperm granulomas to be formed by the body to contain and absorb the sperm which the body treats as a foreign substance.[4]
Effectiveness as birth control
The Royal College of Obstetricians and Gynaecologists state there is a generally agreed upon rate of failure of about 1 in 2000 vasectomies which is considerably better than tubal ligations for which there is one failure in every 200 to 300 cases.[20] Early failure rates, i.e. pregnancy within a few months after vasectomy typically result from having unprotected intercourse too soon after the procedure. Late failure, i.e. pregnancy after recanalization of the vasa deferentia, has been documented.[21] A 2005 systematic review of 28 studies described a total of 183 failures or recanalizations from approximately 43,642 vasectomy patients (0.4%), and 20 studies in the same review described 60 pregnancies after 92,184 vasectomies (0.07%).[22]
Most physicians and surgeons who perform vasectomies recommend one (sometimes two) post-procedural semen specimens to verify a successful vasectomy; however many men fail to return for verification tests citing inconvenience, embarrassment, death, or change in partner.[23] In January 2008 the FDA cleared a home test called SpermCheck Vasectomy[24] that allows patients to perform postvasectomy confirmation tests themselves; however compliance for postvasectomy semen analysis in general remains low.
Complications of vasectomy
Short-term complications include temporary bruising and bleeding, known as hematoma. The primary long-term complications are chronic pain conditions or syndromes that can affect any of the scrotal, pelvic and/or lower-abdominal regions, known as post-vasectomy pain syndrome. Animal and human data indicate that vasectomy does not increase atherosclerosis and that increases in circulating immune complexes after vasectomy are transient. Furthermore, the weight of the evidence regarding prostate and testicular cancer suggests that men with vasectomy are not at increased risk of these cancers.[25]
Post-vasectomy pain syndrome
Main article: post-vasectomy pain syndromePost-vasectomy pain syndrome (PVPS) is a chronic and sometimes debilitating condition that may develop immediately or several years after vasectomy.[26] One survey cites studies that estimate incidence at one case every ten to thirty vasectomies.[27] The pain can be constant orchialgia or epididymal pain, or it can be pain that occurs only at particular times such as with intercourse, ejaculation, or physical exertion.[4]
Vasectomy reversal
Main article: Vasectomy reversalAlthough men considering vasectomies should not think of them as reversible, and most men and their partners are satisfied with the operation,[28] [29] there is a surgical procedure to reverse vasectomies using vasovasostomy (a form of microsurgery first performed by Earl Owen in 1971[30][31]). Vasovasostomy is effective at achieving pregnancy in only 50%-70% of cases, and it is costly, with total out-of-pocket costs in the United States often upwards of $10,000.[32] The rate of pregnancy depends on such factors as the method used for the vasectomy and the length of time that has passed since the vasectomy was performed. The reversal procedures are frequently impermanent, with occlusion of the vas recurring two or more years after the operation. After reversal, sperm counts and motility are usually much lower than pre-vasectomy levels. There is evidence that men who have had a vasectomy may produce more abnormal sperm, which would explain why even a mechanically successful reversal does not always restore fertility.[33][34] The higher rates of aneuploidy and diploidy in the sperm cells of men who have undergone vasectomy reversal may lead to a higher rate of birth defects.[33]
Conceiving after vasectomy
In order to allow the possibility of reproduction via artificial insemination after vasectomy, some men opt for cryostorage of sperm before sterilization.
The cost of Cryo-preservation (Sperm Banking) itself may also be substantially less (approximately $500 every 5 years) than alternative Vaso-vasectomy procedure(s), (est surgery cost of $10,000); however the costs of In-vitro fertilization which are rarely below $10,000 US, and usually run between $12–15,000 US, must be considered. Those interested may want to research and consider the statistical cost/risk/success factors when choosing either of these methods.
Intracytoplasmic sperm injection: Sperm can be aspirated from the testicles or the epididymis, and while there is not enough for successful artificial insemination, there is enough to fertilize an ovum by ICSI. This avoids the problem of anti-sperm antibodies and may result in a faster pregnancy. IVF (In-vitro fertilization) may be less costly (see aforementioned text) per cycle than reversal in some healthcare systems, but a single IVF cycle is often insufficient for conception. Disadvantages include the need for procedures on the woman, and the standard potential side-effects of IVF for both the mother and the child.[35]
Psychological impact
A review of the psychological impact of vasectomy was done on vasectomized men.[36] Informal postoperative surveys indicated that sexual behavior, happiness and the satisfaction of having the procedure done was generally high. In studies that employed psychological tests, and/or interviews from a clinical standpoint, a different overall conclusion emerged. Men were willing to verbally express satisfaction with the procedure, but when questions relating to their perceptions of themselves after the procedure were asked, it became clear that a large number of men had some concern about the long-term consequences of having had the procedure. Furthermore, the psychological impact of being rendered sterile weighed heavy on the majority of participants. In short, a high percentage of men struggle emotionally at some level, and at some point, with the idea of being permanently sterile, but, they remain satisfied with the decision, from the standpoint of having had a successful vasectomy.
Prevalence
Vasectomy is the most effective permanent form of birth control available to men. In nearly every way that vasectomy can be compared to tubal ligation, it is/has a more positive outlook. Vasectomy is more cost effective, less invasive, has techniques that are emerging that may facilitate easier reversal, and has a much lower risk of post operative complications. Given the aforementioned, in the United States,[37] vasectomy is utilized at less than half the rate the alternative female "tubal ligation". According to the research, vasectomy is least utilized among black and Latino populations, groups of which have highest rates of female sterilization.[37]
Tourism
Medical Tourism is likely to be used for expensive and more complicated surgeries; however vasectomy is on the list of available procedures. Men who opt for vasectomy with this method (or more likely, vasectomy reversal) would likely combine their convalesce in/with a vacation-type setting. There are a large number of overseas hospitals whose websites list vasectomy as one of their qualified surgical procedures. Medical tourism is gaining popularity (especially with higher-cost surgeries) as the overall cost of care in developing countries can provide a combination of high-tech medical care at a cost that allows for more enjoyable recovery in a vacation-type setting. Medical tourism is somewhat controversial, and has come under the scrutiny of some governments the concerns of which include quality of care, and post-operative care.[38]
History
The first recorded vasectomy was performed on a dog in 1823.[39] A short time after that, R. Harrison of London performed the first human vasectomy; however the surgery was not done for sterilization purposes, but to bring about atrophy of the prostate. Vasectomy began to be regarded as a method of birth control during the Second World War. The first vasectomy program on a national scale was launched in 1954 in India.
Availability and legality
Vasectomy costs are (or may be) covered in different countries, as a method of both birth control or population control, with some offering it as a part of a national health insurance.
The legality of (and the availability of) a vasectomy may be different from country to country.
See also
References
- ^ Popenoe P (1934). "The progress of eugenic sterilization". Journal of Heredity 25 (1): 19. http://www.eugenicsarchive.org/html/eugenics/static/images/2287.html.
- ^ Cook, Lynley A.; Pun, Asha; Gallo, Maria F; Lopez, Laureen M; Van Vliet, Huib AAM (2007). "Scalpel versus no-scalpel incision for vasectomy". In Cook, Lynley A.. Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD004112.pub3.
- ^ Cook, Lynley A.; Pun, Asha; Gallo, Maria F; Lopez, Laureen M; Van Vliet, Huib AAM (2007). "Scalpel versus no-scalpel incision for vasectomy". In Cook, Lynley A.. Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD004112.pub3.
- ^ a b c Christiansen C, Sandlow J (2003). "Testicular Pain Following Vasectomy: A Review of Post vasectomy Pain Syndrome". Journal of Andrology 24 (3): 293–8. PMID 12721203. http://www.andrologyjournal.org/cgi/content/full/24/3/293.
- ^ a b Weiss, RS; Li, PS (2005). "No-needle jet anesthetic technique for no-scalpel vasectomy". The Journal of urology 173 (5): 1677–80. doi:10.1097/01.ju.0000154698.03817.d4. PMID 15821547.
- ^ http://www.vasectomy-information.com/moreinfo/recanalisation.htm
- ^ Sokal, David; Irsula, Belinda; Hays, Melissa; Chen-Mok, Mario; Barone, Mark A; Investigator Study, Group (2004). "Vasectomy by ligation and excision, with or without fascial interposition: a randomized controlled trial ISRCTN77781689". BMC Medicine 2: 6. doi:10.1186/1741-7015-2-6. PMC 406425. PMID 15056388. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=406425.
- ^ a b Cook, Lynley A.; Van Vliet, Huib AAM; Lopez, Laureen M; Pun, Asha; Gallo, Maria F (2007). "Vasectomy occlusion techniques for male sterilization". In Cook, Lynley A.. Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD003991.pub3.
- ^ Levine, LA; Abern, MR; Lux, MM (2006). "Persistent motile sperm after ligation band vasectomy". The Journal of urology 176 (5): 2146–8. doi:10.1016/j.juro.2006.07.028. PMID 17070280.
- ^ http://www.imccoalition.org/newsletter/2008_August_public.htm
- ^ a b http://www.vasweb.com/vasclip.htm[unreliable medical source?]
- ^ http://www.pro-vas.com/[unreliable medical source?]
- ^ http://www.malecontraceptives.org/methods/shug.php#refs
- ^ http://malecontraceptives.org/methods/mpu.php
- ^ Nielsen CM, Genster HG (1980). "Male sterilization with vasectomy. The effect of the operation on sex life". Ugeskr Laeger 142 (10): 641–643. PMID 7368333.
- ^ Dias, P. L. R. (1983). "The long-term effects of vasectomy on sexual behaviour". Acta Psychiatrica Scandinavica 67 (5): 333–338. doi:10.1111/j.1600-0447.1983.tb00350.x. PMID 6869041.
- ^ Hattikudur, S.; Shanta, S. RAO; Shahani, S.K.; Shastri, P.R.; Thakker, P.V.; Bordekar, A.D. (2009). "Immunological and Clinical Consequences of Vasectomy*". Andrologia 14 (1): 15–22. doi:10.1111/j.1439-0272.1982.tb03089.x. PMID 7039414.
- ^ Deshpande RB, Deshpande J, Mali BN, Kinare SG (1985). "Vasitis nodosa (a report of 7 cases)". J Postgrad Med 31 (2): 105–8. PMID 4057111. http://www.jpgmonline.com/article.asp?issn=0022-3859;year=1985;volume=31;issue=2;spage=105;epage=8;aulast=Deshpande.
- ^ Hirschowitz, L; Rode, J; Guillebaud, J; Bounds, W; Moss, E (1988). "Vasitis nodosa and associated clinical findings". Journal of Clinical Pathology 41 (4): 419–423. doi:10.1136/jcp.41.4.419. PMC 1141468. PMID 3366928. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1141468.
- ^ Royal College of Obstetricians and Gynaecologists. "Sterilisation for women and men: what you need to know". http://www.rcog.org.uk/womens-health/clinical-guidance/sterilisation-women-and-men-what-you-need-know#how.
- ^ Philp, T; Guillebaud, J; Budd, D (1984). "Late failure of vasectomy after two documented analyses showing azoospermic semen". BMJ 289 (6437): 77–79. doi:10.1136/bmj.289.6437.77. PMC 1441962. PMID 6428685. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1441962.
- ^ Griffin, T; Tooher, R; Nowakowski, K; Lloyd, M; Maddern, G (2005). "HOW LITTLE IS ENOUGH? THE EVIDENCE FOR POST-VASECTOMY TESTING". The Journal of Urology 174 (1): 29–36. doi:10.1097/01.ju.0000161595.82642.fc. PMID 15947571.
- ^ Christensen, R. E.; Maples, D. C. (2005). "Postvasectomy Semen Analysis: Are Men Following Up?". The Journal of the American Board of Family Medicine 18: 44–47. doi:10.3122/jabfm.18.1.44.
- ^ Klotz, Kenneth L.; Coppola, Michael A.; Labrecque, Michel; Brugh, Victor M.; Ramsey, Kim; Kim, Kyung-ah; Conaway, Mark R.; Howards, Stuart S. et al. (2008). "Clinical and Consumer Trial Performance of a Sensitive Immunodiagnostic Home Test That Qualitatively Detects Low Concentrations of Sperm Following Vasectomy". The Journal of Urology 180 (6): 2569–2576. doi:10.1016/j.juro.2008.08.045. PMC 2657845. PMID 18930494. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2657845.
- ^ Schwingl, Pamela J; Guess, Harry A (2000). "Safety and effectiveness of vasectomy". Fertility and Sterility 73 (5): 923–936. doi:10.1016/S0015-0282(00)00482-9. PMID 10785217.
- ^ Nangia, Ajay K.; Myles, Jonathan L.; Thomas, Anthony J. (2000). "VASECTOMY REVERSAL FOR THE POST-VASECTOMY PAIN SYNDROME: : A CLINICAL AND HISTOLOGICAL EVALUATION". The Journal of Urology 164 (6): 1939–1942. doi:10.1016/S0022-5347(05)66923-6. PMID 11061886.
- ^ Potts, Jeannette M. (2008). "Post Vasectomy Pain Syndrome". Genitourinary Pain And Inflammation. Current Clinical Urology. pp. 201–209. doi:10.1007/978-1-60327-126-4_13. ISBN 978-1-58829-816-4.
- ^ Landry E, Ward V (1997). "Perspectives from Couples on the Vasectomy Decision: A Six-Country Study" (PDF). Reproductive Health Matters (special issue): 58–67. http://pdf.dec.org/pdf_docs/Pnacq010.pdf.
- ^ Jamieson, D (2002). "A comparison of women's regret after vasectomy versus tubal sterilization". Obstetrics & Gynecology 99 (6): 1073–1079. doi:10.1016/S0029-7844(02)01981-6.
- ^ "About Vasectomy Reversal". Professor Earl Owen's homepage. http://www.earlowen.com.au/about%20vasectomy%20reversal.htm. Retrieved 2007-11-29.
- ^ Owen ER (1977). "Microsurgical vasovasostomy: a reliable vasectomy reversal". Urology 167 (2 Pt 2): 1205. doi:10.1016/S0022-5347(02)80388-3. PMID 11905902.
- ^ Vasectomy Reversal http://www.epigee.org/guide/vasectomy_reversal.html
- ^ a b Sukcharoen, Nares; Ngeamvijawat, J; Sithipravej, T; Promviengchai, S (2003). "High sex chromosome aneuploidy and diploidy rate of epididymal spermatozoa in obstructive azoospermic men". Journal of Assisted Reproduction and Genetics 20 (5): 196–203. doi:10.1023/A:1023674110940. PMID 12812463.
- ^ Abdelmassih, V.; Balmaceda, JP; Tesarik, J; Abdelmassih, R; Nagy, ZP (2002). "Relationship between time period after vasectomy and the reproductive capacity of sperm obtained by epididymal aspiration". Human Reproduction 17 (3): 736–740. doi:10.1093/humrep/17.3.736. PMID 11870128.
- ^ Shridharani, Anand; Sandlow, Jay I (2010). "Vasectomy reversal versus IVF with sperm retrieval: which is better?". Current Opinion in Urology 20 (6): 503–509. doi:10.1097/MOU.0b013e32833f1b35. PMID 20852426.
- ^ Bloom, LJ; Houston, BK (1976). "The psychological effects of vasectomy for American men". The Journal of genetic psychology 128 (2d Half): 173–82. PMID 932701.
- ^ a b Shih G, Turok DK, Parker WJ (April 2011). "Vasectomy: the other (better) form of sterilization". Contraception 83 (4): 310–5. doi:10.1016/j.contraception.2010.08.019. PMID 21397087.
- ^ Lunt, Neil; Carrera, Percivil (2010). "Medical tourism: Assessing the evidence on treatment abroad". Maturitas 66 (1): 27–32. doi:10.1016/j.maturitas.2010.01.017. PMID 20185254.
- ^ Leavesley, JH (1980). "Brief history of vasectomy". Family planning information service 1 (5): 2–3. PMID 12336890.
External links
Birth control methods (G02B, G03A) Comparison Behavioral Avoiding vaginal intercourse: Abstinence • Anal sex • Masturbation • Non-penetrative sex • Oral sex
Including vaginal intercourse: Breastfeeding infertility (LAM) • Calendar-based methods (rhythm, etc.) • Fertility awareness • WithdrawalBarrier or
spermicidalHormonal
(formulations)Progestogen-onlyAnti-estrogen Ormeloxifene (Centchroman)Post-intercourse Emergency contraception (pills or copper IUD) (Yuzpe regimen, Ulipristal acetate)Intrauterine device Abortion Sterilization Male genital surgical and other procedures: reproductive system (ICD-9-CM V3 60-64, ICD-10-PCS 0V) Internal Transurethral incision of the prostate · Prostate biopsy (Transrectal biopsy, Transurethral biopsy) · Prostatectomy (Transurethral resection of the prostate, Radical retropubic prostatectomy) · Transurethral microwave thermotherapy · Transurethral needle ablation of the prostate · Brachytherapy (Prostate brachytherapy) · Prostate massage
seminal vesicles: SpermatocelectomyVasectomy · Vasectomy reversal (Vasovasostomy, Vasoepididymostomy)External Circumcision · Penectomy · Penile prosthesis · Preputioplasty
Penile plethysmograph · Postage stamp testTests Medical imaging: Transscrotal ultrasoundCategories:- Sterilization
- Contraception for males
- 1897 introductions
- Male genital surgery
-
Wikimedia Foundation. 2010.
